Инфекции, связанные с оказанием медицинской помощи (ИСМП), лежат тяжелым бременем на мировом сообществе и связаны со значительной заболеваемостью и смертностью среди пациентов. По данным ВОЗ, уровень ИСМП составляет от 3,5–12,0% в странах с высоким уровнем дохода и до 5,7–19,1% в странах с низким уровнем дохода [1, 2]. Исследователи [3] подчеркивают, что еще в допандемический период распространение ИСМП носило эпидемический характер, в результате чего миллионы пациентов ежегодно умирали от последствий, связанных с ИСМП, а материальные издержки исчислялись миллиардами.
Развитие здравоохранения сопровождалось непрерывным поиском средств и способов профилактики ИСМП, и одним из ключевых направлений стало развитие гигиены и антисептики рук медицинского персонала [1, 4, 5]. Начиная с середины 1980-х гг. мытье и антисептика рук стали одними их основополагающих принципов профилактики ИСМП [6, 7]. Значительный вклад в развитие и совершенствование практик обработки рук персонала внесла ВОЗ, специалисты которой методично и последовательно разрабатывали и внедряли в практику единообразные подходы к реализации данной технологии [8, 9]. В настоящее время большинство национальных требований по антисептике рук медицинского персонала строятся на стратегии, включающей в себя 5 компонентов (шагов) [10].
На первый взгляд, гигиена рук – простая и распространенная процедура, но ее соблюдение в медицинских учреждениях всегда было далеко от идеала. Средний уровень соблюдения гигиены рук составляет 40% в странах с высоким уровнем дохода и менее 20% – в странах с низким уровнем дохода, при этом, согласно рекомендациям ВОЗ, уровень соблюдения гигиены рук ниже 60% считается неудовлетворительным [11].
Причины недостаточного соблюдения антисептики рук среди медицинского персонала достаточно разнообразны, но основными являются неукомплектованность персонала и, как следствие, высокая рабочая нагрузка; отсутствие обучения; недостаточная обеспеченность антисептиками, мылом и водой; отсутствие приверженности антисептике среди руководителей [12].
Наиболее важным элементом стратегии по улучшению гигиены рук является проведение образовательных мероприятий среди медицинских работников. Первый глобальный проект по формированию безопасной для пациентов больничной среды проходил под лозунгом «Чистый уход – это безопасный уход» и показал желаемый эффект. Однако для дальнейшего его поддержания и повышения качества медицинских услуг необходимы долгосрочные образовательные меры. Пандемия COVID-19 обострила ситуацию в области гигиены рук и показала высокую необходимость правильного выполнения процедур по антисептике рук и использованию антисептических средств. Одной из дополнительных проблем в период пандемии явился дефицит в медицинских учреждениях спиртосодержащих антисептиков, вызванный широким применением антисептических средств среди населения в целом [13–16].
Многие исследователи отмечают, что медицинские работники в большинстве своем знают правила обработки рук, но осознание того, что в перекрестной передаче возбудителей ИСМП участвуют такие повсеместно распространенные электронные средства, как мобильные телефоны, наблюдалось далеко не у всех. Если антисептика рук осуществлялась в 65,2% случаев после контакта с пациентом и в 54,5% – после контакта с окружением пациента, то мобильные телефоны подвергались обработке только в 13,6% случаев. Дефицит времени, забывчивость, недостаточная осведомленность о стандартных методах дезинфекции и страх повредить электронные устройства при использовании дезинфицирующих средств явились основными причинами плохого соблюдения правил гигиены электронных устройств [17].
Для достижения эффективной антисептики рук немаловажным является соблюдение таких условий, как коротко подстриженные ногти, отсутствие лака на ногтях и искусственных ногтей, отсутствие украшений. Исследование, проведенное в одной из Миланских клиник в 2016–2017 гг. среди сестринского персонала, показало высокий уровень знаний по вопросам антисептики рук (81%), но при этом 64% опрошенных носили украшения на руках во время работы. А исследования, проведенные в тот же период в службе скорой помощи Финляндии, Швеции, Австралии и Дании, установили приверженность медицинских работников к коротким, чистым ногтям без лака и отсутствию украшений в 84 и 62% соответственно [18, 19].
Эпидемиологическая безопасность медицинских технологий может и должна быть стандартизована через санитарное законодательство, порядки и стандарты оказания медицинской помощи, клинические рекомендации по обеспечению эпидемиологической безопасности медицинской помощи, стандартные операционные процедуры [20]. Воспитание осознанной и мотивированной потребности в качественной обработке рук медицинского персонала является чрезвычайно важным в системе мероприятий по недопущению возникновения ИСМП. В России в период пандемии COVID-19 были обновлены требования по антисептике рук персонала медицинских организаций1–2. Однако, несмотря на прилагаемые усилия, проблема антисептики рук персонала и формирования приверженности ей не теряет своей актуальности, особенно в период повышенного риска реализации биологических угроз.
Цель исследования – изучение приверженности сотрудников медицинских организаций гигиене и антисептике рук в допандемический и пандемический периоды и определение факторов, влияющих на формирование негативного отношения к данной технологии.
Материалы и методы
Исследование проведено сотрудниками Урало-Сибирского научно-методического центра по профилактике инфекций, связанных с оказанием медицинской помощи Екатеринбургского НИИ вирусных инфекций ФБУН ГНЦ ВБ «Вектор» Роспотребнадзора совместно с государственным автономным учреждением здравоохранения Свердловской области «Областная детская клиническая больница». Сотрудников медицинской организации включали в исследование на основании личного добровольного согласия каждого сотрудника. Проведение исследования одобрено локальным этическим комитетом ЕНИИВИ ФБУН ГНЦ ВБ «Вектор» Роспотребнадзора (в настоящее время – Федеральное бюджетное учреждение науки «Федеральный научно-исследовательский институт вирусных инфекций «Виром» Федеральной службы по надзору в сфере защиты прав потребителей и благополучия человека), протокол № 3 от 24.06.2022.
Для оценки уровня приверженности гигиене рук и уровня знаний персонала проведено анонимное анкетирование сотрудников в 2012 и в 2021 г. Число участников приведено в разделе «Результаты». Анкеты содержали вопросы как с множественным выбором, так и альтернативные, а также вопросы оценочного характера, сформированные в отдельные блоки: общие данные (пол, возраст, стаж работы, специальность, подразделение); алгоритм проведения антисептики рук в отделении; источники получения и оценка знаний по вопросам антисептики рук; состояние кожных покровов, факторы, ухудшающие состояние кожного покрова, в том числе бытовые условия, применяемый уход; личное отношение к антисептике рук.
Анкетирование сопровождали исследованием уровня контаминации рук:
2012 г. – смывы с рук сотрудников стационара при приходе на работу (п = 46) и после обработки антисептиком (п = 52), а также с их сотовых телефонов на наличие условно-патогенной микрофлоры (УПМ);
2021 г. – смывы с наружной поверхности 2-й пары перчаток сотрудников инфекционного госпиталя (врачи, медицинские сестры, санитарки/уборщики) на наличие SARS-CoV-2 и УПМ (п = 46).
Для отбора смывов использовали стерильные тампоны, которые после взятия пробы погружали в стерильные одноразовые пробирки с 2 мл транспортной среды для вирусов с целью обнаружения РНК SARS-CoV-2 (ООО «Полигем»), а для обнаружения УПМ – в стерильные стеклянные пробирки с 1% пептонной водой. Хранение, подготовку проб к транспортированию и транспортировку осуществляли с соблюдением требований действующих нормативных документов.
Выявление РНК SARS-CoV-2 в образцах проводили методом ПЦР в реальном времени с применением тест-системы «АмплиСенс® Cov-Bat-FL» в соответствии с инструкцией и MP 3.1.0196-20 «Выявление возбудителя COVID-19» в образцах внешней среды. Для выделения нуклеиновых кислот из исследуемых проб использовали набор «РИБО-преп», для проведения обратной транскрипции применяли набор «Реверта-L» (ФБУН «ЦНИИ эпидемиологии» Роспотребнадзора, Москва). Изучение фенотипических свойств УПМ проводили бактериологическим методом с подтверждением чистоты культуры, постановкой биохимических рядов. Оценку антибиотикорезистентности выделенных штаммов проводили с помощью автоматического бактериологического анализатора VITEK® 2 Compact (bioMerieux SA, Франция) и классического полуколичественного диско-диффузионного метода.
В исследовании применяли эпидемиологический (описательно-оценочный и аналитический), молекулярно-биологический (ОТ-ПЦР), бактериологический и статистический методы исследований. Данные представлены в виде абсолютных и относительных величин (%). Статистическую значимость различий оценивали по точечному критерию Фишера (φ). Для оценки вероятности формирования негативного отношения к антисептике рук в зависимости от различных факторов риска составляли четырехпольную таблицу сопряженности, рассчитывали отношение шансов (ОШ) и его 95% доверительный интервал (ДИ). Различия считали статистически значимыми при p ≤ 0,05. Статистическую обработку данных проводили с использованием пакета прикладных программ Microsoft Office 2010, онлайн-ресурса https://medstatistic.ru/, ПС Statistica 10.
Результаты
В исследовании в 2012 г. приняли участие 73 чел., в 2021 г. – 100 чел. трудоспособного возраста от 19 до 60 лет, средний возраст составил 35,97 ± 10,3 года, медиана (Ме) – 34,9 года. 75% респондентов составили женщины, что соответствует специфике работы отрасли.
Основную долю в исследуемых группах составили медицинские сестры и акушерки (64,4 и 49,0%), на втором месте были врачи (19,2 и 40,0%), на третьем – уборщики/санитарки (16,4 и 9,0%). В допандемический период в исследовании преимущественно приняли участие специалисты со стажем работы до 1 года (38,3%), тогда как в пандемический период 45,0% составили работники со стажем 10 лет и более (табл. 1).
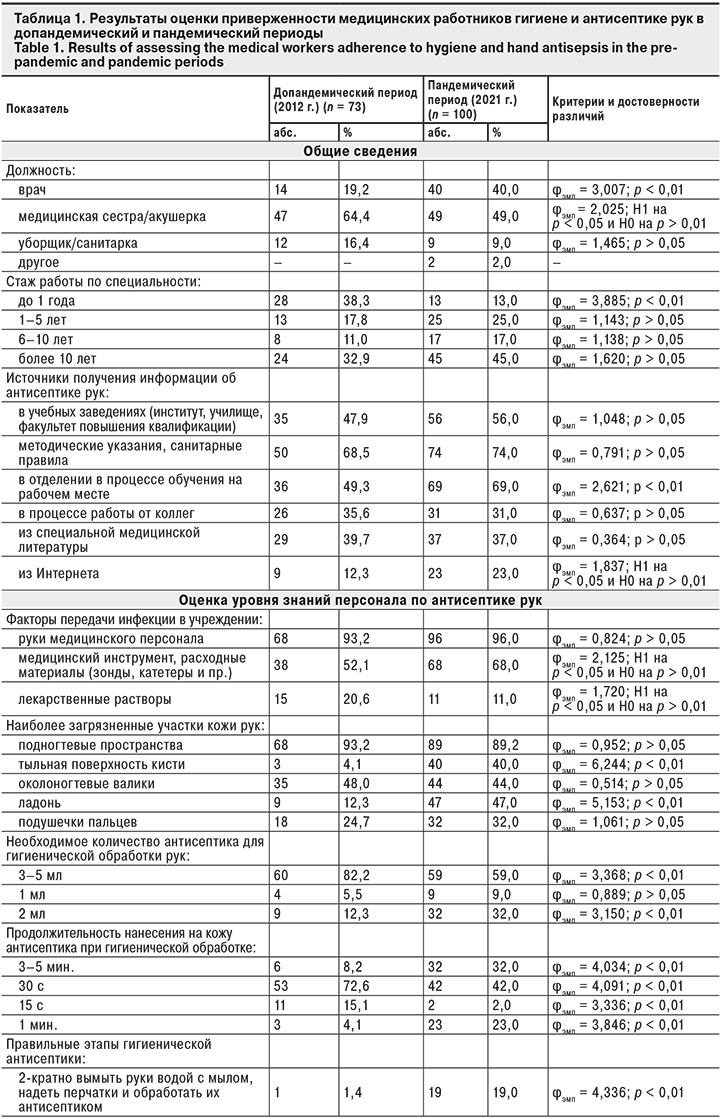
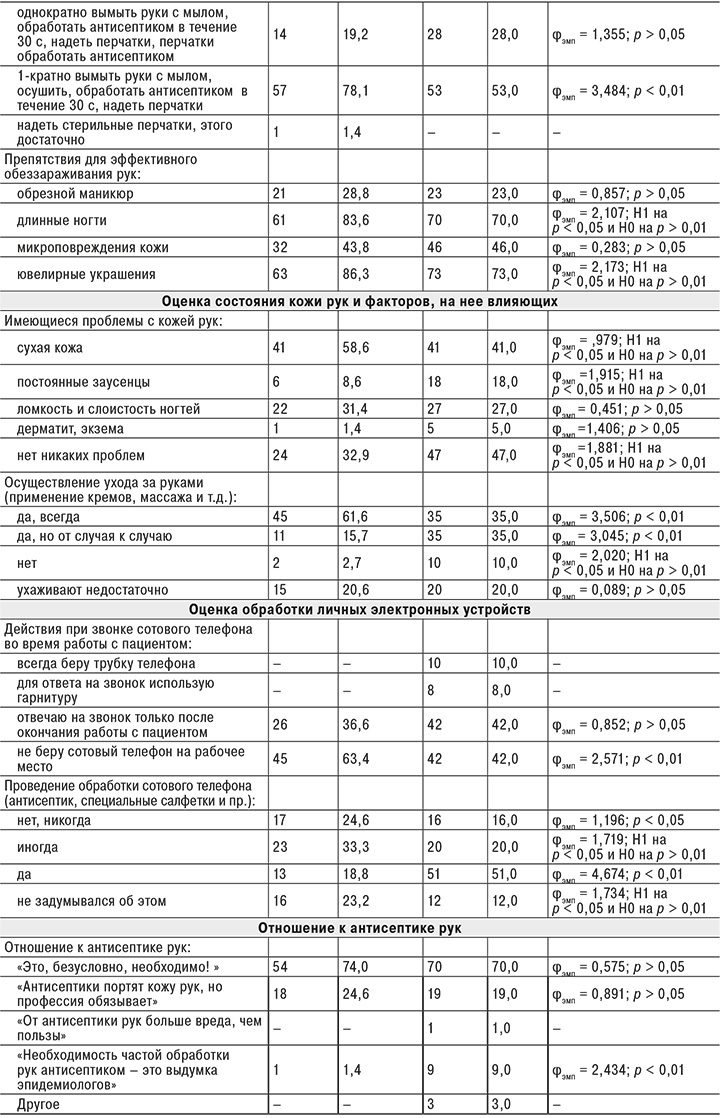
Респонденты указывали, что в процессе профессиональной деятельности они проводят гигиеническую антисептику (90,4 и 98,0%) и хирургическую антисептику рук (68,5 и 47,0%), при этом на наличие бытового уровня обработки (например, мытье рук при приходе на работу или после посещения туалета) указали лишь 31,5 и 23,0% соответственно.
При оценке частоты обработки рук в течение рабочей смены ответ «не считал, но очень часто» выбрали 82,2 и 60,0% респондентов, некоторые указали кратность антисептической обработки рук более детально: до 30 раз в смену – 5,5 и 6,0%, до 20 раз – 2,7 и 19,0%, до 10 раз – 5,5 и 16,0%. Низкую кратность гигиенической антисептики (2–3 раза в течение рабочей смены) отметили 2,7 и 1,0% респондентов соответственно.
Структура источников получения информации об антисептике рук была разнообразна в оба исследуемых периода. Анкетируемые отметили, что для получения информации использовали 2–3 источника, среди которых лидирующее место занимали нормативные документы (68,5 и 74,0%), образовательные программы учебных заведений (47,9 и 56,0%) и образовательные мероприятия на рабочих местах (49,3 и 69,0%). Треть анкетируемых указали, что используют информацию, полученную из специальной медицинской литературы (39,7 и 37,0%), а также от коллег (35,6 и 31,0%). В пандемический период возросла роль Интернет-источников (с 12,3 до 23,0%) и обучения на рабочих местах (с 49,3 до 69,0%).
Уровни знаний персонала в разные периоды изучения были сопоставимы. Так, в качестве ведущих факторов передачи ИСМП респонденты часто указывали руки медицинского персонала (93,2 и 96,0%), но недооценивали роль медицинского инструмента и расходных материалов (52,1 и 68,0%), а также лекарственных растворов (20,6 и 11,0%). Наиболее загрязненными участками кожи рук респонденты справедливо считали подногтевые пространства (93,2 и 89,0%), однако околоногтевые валики и подушечки пальцев были указаны лишь в 30–40% анкет. В то же время до 40,0% анкетируемых считали труднообрабатываемыми тыльную и ладонную поверхность кисти.
Согласно рекомендациям ВОЗ [10], для большинства зарегистрированных в РФ антисептиков необходимым для качественной обработки рук количеством является 5 мл средства. Именно такой вариант ответа был выбран большинством респондентов (82,2 и 59,0%). Однако значительная часть медицинских работников были уверены, что для качественной обработки рук достаточно 2 мл (12,3 и 32,0%) или даже 1 мл (5,5 и 9,0%) антисептического средства. Отмечено, что доля таких ответов в пандемический период значительно увеличилась и составила 41,0% против 17,8% в допандемический период.
Такая же тенденция была характерна при оценке знаний о продолжительности нанесения антисептика на кожу рук. В допандемический период доля респондентов, указавших правильную продолжительность нанесения антисептика (30 с), составила 72,6%, 15-секундный период считали достаточным 15,1%, а 1–3–5-минутный период – 12,3%. В пандемический период снизилась доля лиц, считающих достаточным для обработки рук 30-секундный период, до 42,0% выросла доля респондентов, считающих достаточным 1–3–5-минутный период, – до 55,0%.
В пандемический период значимо изменились представления медицинского персонала об этапности гигиенической антисептики. Так, в допандемический период 78,1% были уверены, что для качественной обработки рук необходимо однократно вымыть руки с мылом, осушить, обработать антисептиком в течение 30 с и надеть перчатки. В пандемический период доля таких лиц снизилась до 53,0%, и выросла доля респондентов, считающих необходимым обработать наружную поверхность перчаток после их надевания (до 47,0%).
Отмечено, что рейтинг событий, препятствующих эффективному обеззараживанию рук, существенно не изменился, и в оба анализируемых периода на 1-м месте было наличие на руках ювелирных украшений (86,3 и 73,0%), на втором – длинных ногтей (83,6 и 70,0%), на третьем – микроповреждений кожи рук (43,8 и 46,0%). Одинаково часто (28,8 и 23,0%) недооценивалось значение обрезного маникюра как варианта микроповреждений кожи рук.
Существенным препятствием для качественной антисептики рук персонала может стать состояние кожи рук. На обоих этапах исследования лишь 30–40% работников указали на отсутствие таких проблем. Остальные отмечали сухость кожи на руках (58,6 и 41,0%), ломкость и слоистость ногтей (31,4 и 27,0%), заусенцы (8,6 и 18,0%), проявления дерматита и экземы (1,4 и 5,0%). При этом постоянный уход за руками осуществляли лишь 61,6% респондентов в допандемический период и 35,0% – в пандемический. Остальные либо не ухаживали за кожей рук (2,7 и 10,0%), либо делали это недостаточно (20,6 и 20,0%) и от «случая к случаю» (15,7 и 35,0%).
За последние 10 лет мобильный телефон утратил значение простого средства коммуникации и стал неотъемлемой частью жизни большинства людей. Для медицинских работников необходимость использования устройств сотовой связи связана не только с многозадачностью современных гаджетов, но и с необходимостью всегда быть на связи. В допандемический период 63,4% респондентов (63,4% предпочитали не брать личный телефон на рабочее место, 36,6% указали, что отвечают на звонок только после окончания работы с пациентом. В пандемический период ситуация несколько изменилась, и доля медицинских работников, не берущих сотовый телефон на рабочее место, снизилась до 42,0%. Остальные респонденты указали, что отвечают на телефонный звонок только после окончания работы с пациентом (42,0%), используют для ответа гарнитуру (8,0%) либо отвечают на входящий звонок в любом случае (10,0%).
При этом обработку личного сотового телефона (ответы «да» и «иногда») проводили 52,1% респондентов в допандемический период и 71,0% – в пандемический. Остальные никогда этого не делали (24,6 и 16,0%) и даже не задумывались об этом (23,2 и 12,0%).
Перечень ситуаций, при которых необходимо проведение антисептической обработки рук, регламентирован нормативными документами1,2. На разных этапах данный перечень несколько отличался, что нашло отражение и в результатах исследования (см. рисунок).
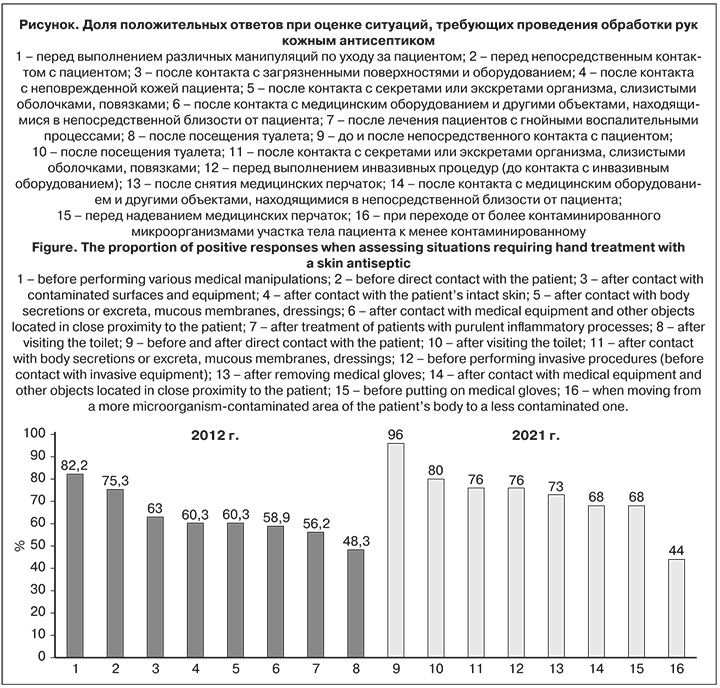
По результатам оценки приверженности антисептике рук в допандемический период 82,2% респондентов считали необходимым провести обработку рук перед выполнением различных манипуляций по уходу за пациентом; 75,3% – перед непосредственным контактом с пациентом; 63,0% – после контакта с загрязненными поверхностями и оборудованием; по 60,3% – после контакта с неповрежденной кожей пациента и после контакта с секретами и экскретами организма, слизистыми оболочками, повязками; 58,9% – после лечения пациентов с гнойными воспалительными процессами; 56,2% – после контакта с медицинским оборудованием и другими объектами, находящимися в непосредственной близости от пациента; 43,8% – после посещения туалета. Суммарный уровень приверженности антисептике рук в допандемический период составил 63,1%.
В пандемический период 96% респондентов считали необходимым провести обработку рук до и после непосредственного контакта с пациентом; 80% – и после посещения туалета; по 76% – после контакта с секретами или экскретами организма и перед выполнением инвазивных процедур; 73% – после снятия медицинских перчаток; по 68% – перед надеванием перчаток и после контакта с оборудованием; 44% – при переходе от более к менее контаминированному участку. Суммарный уровень приверженности антисептике рук в пандемический период составил 72,6%.
В 2012 г. одновременно с анкетированием было проведено микробиологическое исследование смывов с рук и мобильных телефонов. Контаминация рук до антисептической обработки была выявлена в 38,8% проб. Структура выделенных штаммов была разнообразна: Staphylococcus aureus (10; 52,6%), Klebsiella oxytoca (3; 15,8%), Klebsiella pneumoniae (2; 10,5%), Enterobacter cloacae (2; 10,5%), Pseudomonas aeruginosa (1; 5,3%), Enterobacter aerogenes (1; 5,3%).
После проведенной антисептической обработки уровень контаминации рук медицинского персонала значительно снизился (в 4,0 раза), доля нестандартных проб составила 9,6%. Спектр выделенных штаммов был представлен 3 видами УПМ: S. aureus (2; 40%), Ps. aeruginosa (2; 40%), и E. cloacae (1; 20%). С личных мобильных устройств в 11,8% проб был выделен S. aureus, что соответствовало результатам смывов с рук владельцев телефонов.
В 2021 г. при проведении исследования с учетом специфики ситуации был сделан акцент на одновременную оценку вирусно-бактериальной контаминации наружной пары перчаток медицинского персонала. В результате 28,3% исследованных проб были нестандартны, а спектр выделенных возбудителей был представлен УПМ: E. faecalis (5; 33,3%), S. aureus (2; 13,3%), K. pneumoniaе (2; 13,3%), Pantoea agglomerans (ранее – Enterobacter agglomerans) (1; 6,7%) и SARS-CoV-2 (5; 33,3%). В 2 случаях отмечено выделение с наружной поверхности перчаток врачей вирусно-бактериальных ассоциаций, представленных SARS-CoV-2 и E. faecalis (табл. 2).

В завершение исследования респондентам было предложено выбрать фразу об антисептике, наиболее соответствующую их личному отношению к данной технологии. В допандемический и пандемический периоды исследования бóльшая часть респондентов выбрали фразы «Это, безусловно, необходимо» (74,0 и 70,0%) и «Антисептики портят кожу рук, но профессия обязывает» (24,6 и 19,0%), что характеризует высокий уровень приверженности. Однако в период пандемии выросла доля респондентов, выбравших вариант «Необходимость частой обработки рук антисептиком – это выдумка эпидемиологов» (с 1,4 до 9,0%), и появились сотрудники, считающие, что «От антисептики рук больше вреда, чем пользы».
Обсуждение
Причинами недостаточной приверженности антисептике рук могут быть забывчивость персонала, незнание правил обработки рук, недостаточная укомплектованность персоналом и, как следствие, высокая рабочая нагрузка; отсутствие обучения; недостаточная обеспеченность антисептиками, мылом и качественной водой; отсутствие приверженности антисептике среди руководителей [11, 21].
В настоящем исследовании была представлена характеристика приверженности антисептике у медицинского персонала в разные периоды работы медицинских организаций – допандемический и пандемический. Показано, что каждый из периодов имел свои особенности, при этом общей тенденцией являлось сохранение у медицинского персонала высокого уровня приверженности антисептике рук.
Полученные нами данные во многом согласуются с результатами других исследователей. Так, J. Hammerschmidt и соавт. [22] отмечено, что правильное профессиональное отношение к антисептике рук в коллективе формируется под воздействием примера лидеров. Было показано, что для медицинских сестер было важно услышать мнение о гигиене рук от своих коллег – медицинских сестер, а для студентов и младшего медицинского персонала – мнение опытных наставников. В нашем исследовании также отмечен рост значимости обучения на рабочих местах с 49,3% (2012 г.) до 69,0% (2021 г.), что может свидетельствовать об активной вовлеченности административных ресурсов в процесс обучения.
Достоверная и полноценная информация является основой для формирования знаний об антисептике. M.B. Martos-Cabrera и соавт. [23] отмечают, что применение традиционных методов обучения в комплексе с использованием инновационных форм повышают соблюдение правил гигиены рук до 70%. В нашем исследовании установлено, что респонденты использовали в среднем 2–3 различных источника информации об антисептике. За 10-летний период наблюдения отмечено возрастание роли сведений, полученных из Интернет-источников, что следует учитывать в программах формирования приверженности антисептике рук. В то же время в исследовании M. Kielar и соавт. [16] показано, что внедрение дополнительных образовательных мероприятий в учреждении значительно повышает уровень соблюдения гигиены рук, но для дальнейшего поддержания высокого уровня требуется систематическое проведение таких мероприятий.
В исследовании отмечено, что, несмотря на рост значимости обучения персонала на рабочих местах, качество полученных знаний не достигает должного уровня. При оценке уровня теоретических знаний медицинского персонала отмечено понимание значения рук как основного фактора передачи ИСМП и снижение знаний о технологии антисептической обработки рук: необходимое количество антисептика, продолжительность его нанесения, последовательность действий. В 2021 г. 47,0% респондентов посчитали возможным проведение обработки перчаток антисептиком, тогда как в 2012 г. только 20,6% выбрали этот вариант ответа. Кроме того, медицинские работники не всегда правильно определяли ситуации, требующие антисептической обработки рук в соответствии с нормативными документами. В то же время суммарная доля правильных ответов выросла на 9,5%, с 63,1% в 2012 г. до 72,6% в 2021 г. (см. рисунок).
Ряд других исследователей [24, 25] также отмечают улучшение соблюдения правил антисептики рук в период пандемии COVID-19. До пандемии в странах Европы средний уровень соблюдения гигиены рук составлял порядка 40%, в Китае – до 75%. В период пандемии в Китае уровень соблюдения требований по антисептике рук достиг рекордных 96% (Ухань, Китай), в Германии (Бремен) вырос с 47 до 100%. В то же время в ряде европейских стран прогресс был менее значительным (Катания, Италия – 62% в 2016 г. и 66% в 2020 г.).
В целом респондентами продемонстрировано положительное отношение к антисептике рук (в 2012 г. – 74,0%, в 2022 г. – 70,0%), однако выросла доля неоднозначных оценок, формированию которых способствовал ряд факторов:
- наличие высшего медицинского образования, ОШ = 3,273 (95% ДИ 1,347–7,952);
- стаж работы в медицинской организации менее 10 лет, ОШ = 3,273 (95% ДИ 1,347–7,952);
- отсутствие практики обработки личного сотового телефона, ОШ = 3,683 (95% ДИ 1,473–9,212);
- отсутствие навыков ухода за кожей рук, ОШ = 1,641 (95% ДИ 0,428–6,297);
- мужской пол, ОШ = 1,833 (95% ДИ 0,709–4,740);
- самостоятельное изучение специализированной литературы по антисептике рук, ОШ = 2,316 (95% ДИ 0,899–5,963).
L.D. Moore и соавт. [26] в своих исследованиях сделали вывод, что уровень приверженности гигиене рук менялся в зависимости от развития пандемии COVID-19. Так, в начале пандемии он увеличился, затем в течение некоторого времени оставался на постоянном уровне и по мере прогрессирования пандемии снижался, что, возможно, связано с ослаблением контроля и стимулирования медицинского персонала со стороны администрации медицинских организаций [27].
В настоящее время мобильные телефоны являются высокотехнологичными устройствами, которые служат не только для связи между людьми, но и обладают мультифункциональными свойствами. В нашем исследовании показано, что сотрудники медицинских организаций все чаще используют личные сотовые телефоны на рабочих местах (в 2012 г. – 36,6%, в 2021 г. – 58,0%), при этом 28% по-прежнему не обрабатывают гаджеты и даже не задумываются об этом.
Суммарный уровень контаминации кожи рук, средств индивидуальной защиты и телефонов медицинского персонала был достаточно высоким и в условиях пандемии COVID-19 имел выраженную тенденцию к росту с 22,0% (2012 г.) до 28,3% (2021 г.), что согласуется с результатами других исследователей. По оценке E.P.S. Espinoza и соавт. [28], большинство медицинских работников считали мобильные телефоны источником перекрестной передачи патогенов в условиях медицинского учреждения, а проведенные лабораторные исследования смывов с поверхности телефонов выявили наличие РНК SARS-CoV-2, что свидетельствует о необходимости разработки универсальной политики использования девайсов в условиях медицинских организаций и проведении их регулярной обработки [17, 29, 30].
Медицинские работники относятся к группе риска по развитию профессиональных кожных заболеваний, распространенность которых оценивается в 30% [31]. В период пандемии COVID-19 наиболее распространенными признаками поражения кожи рук были сухость (55,7%), зуд (31,2%) и сыпь (23,0%) [32, 33]. В нашем исследовании показано, что медработников беспокоили сухая кожа, ломкость и слоистость ногтей, заусенцы и проявления дерматита/экземы.
Отмечено, что уход за кожей рук осуществляла лишь 1/3 респондентов (в 2012 г. – 61,6%, в 2021 г. – 35,0%). 20–28% сотрудников в бытовых условиях контактировали с вредными для кожи рук факторами (агрессивные химические соединения, работа с землей и пр.), а частота применения перчаток при этом составила 10–50% в зависимости от вида выполняемых работ (уборка помещений – 50,0%, мытье посуды – 25,0%, ремонт автомобиля – 23,0%, работа на садовом участке – 21,0%, ручная стирка белья – 8,0%). При этом 75,0% респондентов считали, что именно профессиональные факторы (гигиена и антисептика рук) являются ведущими в повреждающем действии на кожу рук.
Сравнение данных о приверженности антисептике рук в разных странах показывает, что достаточное соблюдение правил обработки рук, несмотря на огромные успехи в изучении и внедрении различных программ до настоящего времени, имеет ряд проблем. При этом хорошие результаты показывают учреждения, где стимулируется соблюдение требований и налажена обратная связь, но в настоящее время в долгосрочной перспективе не известна эффективность этих мероприятий, так как добиться устойчивого успеха оказывается очень трудно [34, 35].
Заключение
Несмотря на преимущественно положительное отношение к антисептике рук, отмечен рост доли неоднозначных оценок, формированию которых способствовали наличие высшего медицинского образования, стаж работы в медицинской организации менее 10 лет, отсутствие практики обработки личного сотового телефона и навыков ухода за кожей рук. Влияние ряда факторов, таких как мужской пол и самостоятельное изучение специализированной литературы по антисептике рук, требует дополнительного изучения.
Суммарный уровень знаний о ситуациях, требующих проведения антисептической обработки рук, вырос. В то же время результаты проведенных лабораторных исследований смывов с рук и наружных поверхностей перчаток медицинского персонала продемонстрировали высокий уровень вирусно-бактериальной контаминации, что способствует созданию условий для циркуляции вирусных и бактериальных патогенов в медицинской организации.


