Известно, что SARS-CoV-2 приводит к более тяжелому течению инфекции у определенных групп, особенно у пожилых людей, проживающих в домах престарелых [1, 2]. По результатам исследования, проведенного в Китае, у 81% населения за пределами закрытых учреждений длительного ухода (ЗУДУ) заболевание протекает в легкой форме, у 14% – в среднетяжелой и лишь у 5% COVID-19 протекает тяжело, с серьезными осложнениями в виде острой дыхательной недостаточности, септического шока и полиорганной недостаточности [2]. Так как проживающие в ЗУДУ – особо уязвимая группа населения, неотложная медицинская помощь (например, искусственная вентиляция легких) требуется почти 54,5% заболевших, а доля умерших в одном очаге достигала 36,1% [3, 4]. Поскольку эти лица нуждаются в постоянном постороннем уходе, страдают многочисленными хроническими заболеваниями и психическими расстройствами, смертность среди них вносила существенный вклад в общую смертность от коронавируса [5–15].
Многие исследователи показали, что мужской пол, пожилой возраст, сахарный диабет 2-го типа, ожирение, деменция, хроническая обструктивная болезнь легких, злокачественные новообразования, депрессия, фибрилляция предсердий и артериальная гипертензия (АГ) являются предикторами тяжелого течения COVID-19 [16–23]. Некоторые авторы включают в перечень факторов риска недержание кишечника, большое число сопутствующих заболеваний и болезнь Паркинсона [20–22].
Для смягчения последствий пандемии среди проживающих в ЗУДУ необходимо проводить исследования факторов риска, влияющих на эпидемический процесс в этой уязвимой группе населения.
Цель исследования – оценка шансов развития пневмонии и шансов летального исхода у заболевших COVID-19 проживающих в ЗУДУ в зависимости от возраста, пола, группы инвалидности, сопутствующих заболеваний и их числа, функционального статуса и построение прогностической модели вероятности развития пневмонии и вероятности летального исхода.
Материалы и методы
Проведен анализ 355 историй болезни и посмертных эпикризов проживающих в домах престарелых, геронтологических центрах, домах ветеранов и социальных домах на территории Москвы, заболевших COVID-19 в период с 2020 по 2022 г.
Факторы риска при COVID-19 были изучены нами в исследовании «случай–контроль».
Дизайн исследования «случай–контроль» для оценки шансов развития пневмонии
Группа «случай» включала 248 лиц, проживающих в ЗУДУ, с инфекцией, вызванной SARS-CoV-2. Критерии включения: основной диагноз U07.1, заболевание средней или тяжелой степени тяжести, наличие пневмонии. Критерии исключения: отсутствие сведений о развитии пневмонии в связи с U07.1. Группа «контроль» включала 107 участников, проживающих в ЗУДУ, с инфекцией, вызванной SARS-CoV-2. Критерии включения: основной диагноз – U07.1, легкое или бессимптомное течение заболевания, отсутствие пневмонии. Критерии исключения: отсутствие сведений о тяжести течения, летальный исход в связи с U07.1 (в случае атипичного и бессимптомного течения болезни).
Дизайн исследования «случай–контроль» для оценки шансов летального исхода
Группа «случай» включала 68 лиц, проживающих в ЗУДУ, с инфекцией, вызванной SARS-CoV-2. Критерии включения: основной диагноз – U07.1 тяжелой степени, смерть от любых причин. Критерии исключения: отсутствие сведений об исходе заболевания. Группа «контроль» включала 287 участников, проживающих в ЗУДУ, с инфекцией, вызванной SARS-CoV-2. Критерии включения: основной диагноз – U07.1, выписка пациента с выздоровлением. Критерии исключения: отсутствие сведений об исходе заболевания.
В качестве факторов риска развития пневмонии и летального исхода заболевания у проживающих в ЗУДУ были рассмотрены следующие характеристики заболевших: возраст, пол, сопутствующие заболевания и их число, возможность передвигаться без посторонней помощи, группа инвалидности, нарушение тазовых функций (недержание мочеиспускания и дефекации).
В число сопутствующих входили:
1) заболевания сердечно-сосудистой системы: ишемическая болезнь сердца (ИБС), нарушения сердечного ритма, легочное сердце, гипертоническая болезнь (ГБ), тромбоз, сердечная недостаточность, порок сердца, хроническая ишемия нижних конечностей;
2) заболевания органов дыхания: туберкулез, хронический бронхит, хроническая обструктивная болезнь легких, эмфизема легких, бронхиальная астма, пневмофиброз;
3) эндокринные заболевания: гипотиреоз или гипертиреоз, сахарный диабет;
4) нейродегенеративные заболевания: шизофрения; деменция или умственная отсталость; ДЦП; эпилепсия или эписиндром; болезни Альцгеймера и Паркинсона;
5) другие заболевания: онкологические, нефропатии, анемия, ВИЧ-инфекция, вирусные гепатиты, пролежни, ожирение или кахексия, микоз всего тела, хронический гастрит, хронический панкреатит.
Использовали сведения о группах инвалидности только из медицинской документации ЗУДУ, аналогичные сведения из документации стационаров не учитывали. III группа инвалидности не оценивали как прогностический признак развития пневмонии или летального исхода из-за небольшой выборки (всего 5 чел.).
Сведения о нарушениях или нормальной работе тазовых органов брали из амбулаторных карт ЗУДУ и из документации стационаров.
Вакцинацию как вероятный фактор профилактики осложнения течения СOVID-19 не рассматривали по причине почти 100% охвата иммунизацией в Москве лиц, проживающих в ЗУДУ1.
ЗУДУ предназначены для проживания и обслуживания лиц пожилого возраста и инвалидов старше 18 лет. В исследуемую выборку лица младше 18 лет не входили.
Статистический анализ проводили с использованием программы StatTech v. 2.6.5. Количественные показатели оценивали на предмет соответствия нормальному распределению с помощью критерия Колмогорова–Смирнова. При отсутствия нормального распределения их описывали с помощью медианы (Me) и нижнего и верхнего квартилей [Q1–Q3)]. Сравнение двух групп по количественному показателю, распределение которого отличалось от нормального, выполняли с помощью U-критерия Манна–Уитни. Для сравнения процентных долей при анализе четырехпольных таблиц сопряженности применяли критерий χ2 Пирсона.
Построение прогностической модели вероятности определенного исхода выполняли методом бинарной логистической регрессии. При этом мы принудительно включали факторы, представленные в табл. 1 и 2. Были отобраны предикторы, которые после учета влияния потенциальных искажающих факторов (конфаундеров) создавали наиболее эффективную модель с наивысшей прогностической силой, выражающейся в чувствительности и специфичности модели и площади под ROC-кривыми.
Результаты
Группа заболевших, по которой мы оценивали факторы риска развития пневмонии и факторы риска летального исхода при заболевании COVID-19, состояла из 355 чел., соответствующих критериям включения, из них 168 (47%) мужчин и 187 (53%) женщин.
Ме возраста мужчин составила 63 года (48–71), Ме возраста женщин была более чем на 10 лет выше и составила 74 года (63–83). (p < 0,001). Ме числа сопутствующих заболеваний у мужчин была достоверно ниже, чем у женщин: соответственно 4 (2–6) и 5 (4–7) (p < 0,001). Мужчины в нашем исследовании II группу инвалидности имели в 1,865 раза чаще, чем женщины (p = 0,007), они могли самостоятельно ходить в 3,792 раза чаще (p < 0,001).
Структура сопутствующей патологии у заболевших COVID-19 лиц, проживающих в ЗУДУ, представлена на рис. 1.
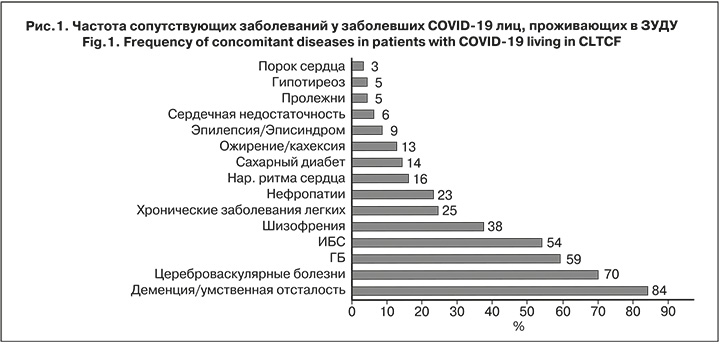
Среднее число сопутствующих заболеваний было равно 5: от 1 до 4 – у 41,9% заболевших, от 5 до 9 – у 51,2%, от 10 до 16 – у 6,7%.
Группу инвалидности имели все 355 чел., информация о группе инвалидности была на 315 чел.: у 157 чел. (51%) была I группа, у 153 (48%) – II группа, у 5 (1%) – III группа.
Информация о наличии или отсутствии нарушений тазовых функций имелась на 137 чел., из них 78 (57%) страдали недержанием.
В группе заболевших лица с летальным исходом (тяжелая форма заболевания) составили 19%, лица с осложнением COVID-19 в виде пневмонии (без летального исхода, средняя степень тяжести) – 50%, перенесли заболевание в легкой или бессимптомной форме (легкая степень тяжести) – 31%.
Факторы риска развития пневмонии
В зависимости от осложнения пневмонии больные были разделены на группу «случай» (с пневмонией, n = 248) и группу «контроль» (без пневмонии, n = 107). В исследовании «случай–контроль» оценивали факторы риска тяжелого течения COVID-19 (табл. 1).
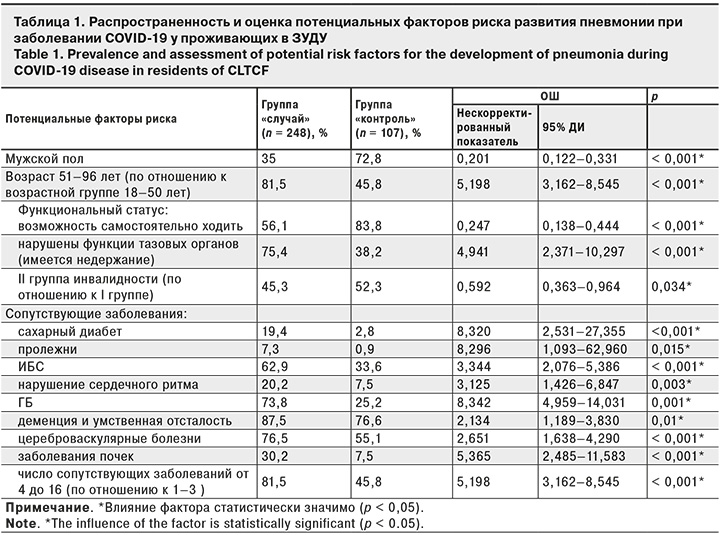
В результате проведенной бинарной логистической регрессии и с учетом влияния потенциальных искажающих факторов (конфаундеров) было установлено, что шанс развития пневмонии при заболевании COVID-19 у проживающих в ЗУДУ:
- увеличивается в 1,037 раза с увеличением возраста на 1 год (по сравнению с возрастом 18 лет) [скорректированный показатель ОШ 1,037 (95% ДИ 1,015–1,059; p = 0,001)];
- уменьшается в 3,194 раза у мужчин [скорректированный показатель ОШ 0,313 (95% ДИ 0,163–0,599; p < 0,001)];
- увеличивается в 1,268 раза с увеличением числа сопутствующих заболеваний на 1 [скорректированный показатель ОШ 1,268 (95% ДИ 1,089–1,478: p = 0,002)];
- уменьшается в 2,169 раза среди лиц со II группой инвалидности (по сравнению с I группой) [скорректированный показатель ОШ 0,461 (95% ДИ 0,236–0,900; p = 0,023)];
- увеличивается в 2,638 раза у лиц с гипертонической болезнью (ГБ) [скорректированный показатель ОШ 2,638 (95% ДИ 1,175–5,918; p = 0,019)].
Нами была разработана прогностическая модель для определения вероятности развития пневмонии в зависимости от возраста, пола, группы инвалидности, числа сопутствующих заболеваний, наличия ГБ методом бинарной логистической регрессии. Число наблюдений составило 310. Наблюдаемая зависимость выражена уравнением:
P = 1 / (1 + е-z) × 100%
z = -1,840 + 0,036XВ - 1,163XМ - 0,775XГИ+ 0,238XЧСЗ + 0,970XГБ,
где P – вероятность развития пневмонии;
XВ – возраст;
XМ – мужской пол;
XГИ – группа инвалидности (0 – I группа, 1 – II группа);
XЧСЗ – число сопутствующих заболеваний;
XГБ – ГБ (0 – нет, 1 – есть).
Полученная регрессионная модель является статистически значимой (p < 0,001). Исходя из значения коэффициента детерминации Найджелкерка, она объясняет 47,3% наблюдаемой дисперсии показателя «Пневмония».
С помощью ROC-анализа было определено оптимальное значение прогностической функции Р (рис. 2).

Площадь под ROC-кривой составила 0,866 ± 0,020 (95% ДИ 0,827–0,905). Полученная модель была статистически значимой (p < 0,001). Чувствительность и специфичность модели составили 74,3 и 84,4%, соответственно.
Факторы риска летального исхода
Заболевшие были разделены на 2 группы: «случай» – с летальным исходом (n = 68) и «контроль» – без летального исхода (n = 287). В исследовании «случай–контроль» мы оценивали факторы риска тяжелого течения COVID-19 с летальным исходом (табл. 2).
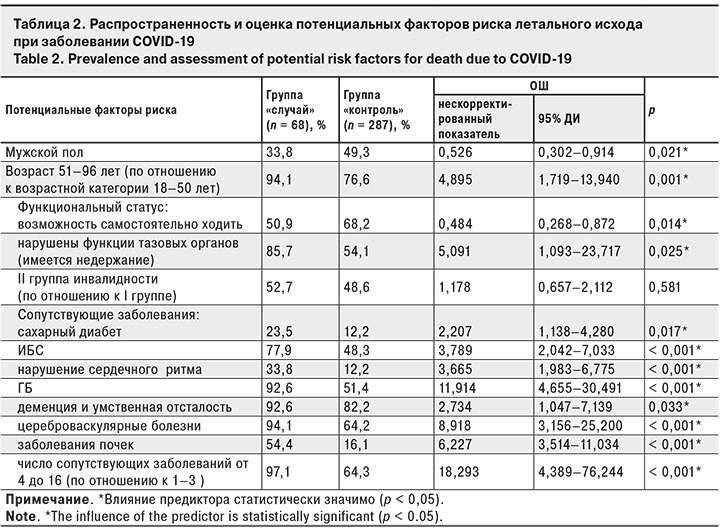
В результате проведенной бинарной логистической регрессии с принудительным включением предикторов и с учетом влияния потенциальных искажающих факторов (конфаундеров) было установлено, что шанс смерти при заболевании COVID-19 у проживающих в ЗУДУ увеличивается:
- в 1,045 раза с увеличением возраста на 1 год (по сравнению с возрастом 18 лет) [скорректированный показатель ОШ 1,045 (95% ДИ 1,016–1,076; p = 0,002)];
- в 1,096 раза с увеличением числа сопутствующих заболеваний на 1 [скорректированный показатель ОШ 1,096 (95% ДИ 0,953–1,260; p = 0,198)];
- в 3,808 раза при наличии нефропатии, [скорректированный показатель ОШ 3,808 (95% ДИ 1,861–7,791; p < 0,001)];
- в 3,758 раза при наличии ГБ [скорректированный показатель ОШ 3,758 (95% ДИ 1,281–11,012; p = 0,016)].
Нами была разработана прогностическая модель для определения вероятности умереть у заболевших COVID-19 лиц, проживающих в ЗУДУ, в зависимости от возраста, числа сопутствующих заболеваний, ГБ, заболеваний почек методом бинарной логистической регрессии. Число наблюдений составило 354. Наблюдаемая зависимость описывается уравнением:
P = 1 / (1 + e-z) × 100%
z = -6,637 + 0,044XВ + 0,91XЧСЗ+ 1,324XГБ + 1,337XЗП,
где P – вероятность летального исхода;
XВ – возраст;
XЧСЗ – число сопутствующих заболеваний;
XГБ – ГБ (0 – нет, 1 – есть);
XЗП – заболевания почек (0 – нет, 1 – есть).
Полученная регрессионная модель является статистически значимой (p < 0,001). Исходя из значения коэффициента детерминации Найджелкерка, модель объясняет 35,2% наблюдаемой дисперсии показателя «Летальный исход».
При оценке зависимости вероятности летального исхода от значения логистической функции P с помощью ROC-анализа была получена следующая кривая (рис. 3).
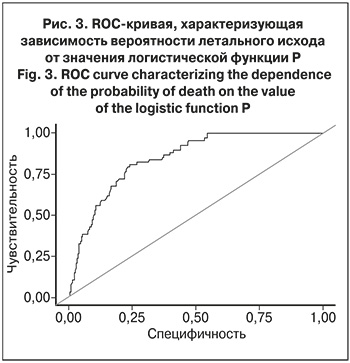
Площадь под ROC-кривой составила 0,843 ± 0,031 (95% ДИ 0,812–0,874; p < 0,001). чувствительность и специфичность модели – 80,9 и 75,9%, соответственно.
Обсуждение
Многочисленные литературные источники [19, 22, 23] относят мужской пол в данных коллективах к факторам риска развития неблагоприятных исходов заболеваний, однако в нашем исследовании мужской пол оказался протективным фактором, снижающим шанс развития пневмонии в 4,977 раза и летального исхода в 1,9 раза. Вместе с тем, Ме возраста мужчин, заболевших пневмонией, составила 68 (62–75) лет и была достоверно ниже, чем Ме возраста женщин с пневмонией, которая составила 77 (67–83) лет (p < 0,001), а средний возраст мужчин с летальным исходом составил 70,39 года и был достоверно ниже, чем средний возраст умерших женщин – 81,04 года (p < 0,05).
Данные результаты можно объяснить тем, что мужчины попадают в социальные дома Москвы на постоянное проживание с различными психоневрологическими расстройствами в более молодом возрасте и в более высоком функциональном статусе, чем женщины.
Полученные прогностические модели можно оценить как очень хорошего качества и имеющие высокую прогностическую силу, если оценивать их по чувствительности и специфичности, площади под ROC-кривой и коэффициенту детерминации Найджелкерка [25].
Заключение
При анализе факторов риска было установлено, что сопутствующие заболевания (сахарный диабет, ИБС, нарушение сердечного ритма, ГБ, деменция и умственная отсталость, цереброваскулярные болезни, заболевания почек) и их большое число, пожилой и старший возраст, низкий функциональный статус (недержание кала и мочи, I группа инвалидности) были ассоциированы с развитием пневмонии и летальным исходом у проживающих в ЗУДУ, тогда как мужской пол и возможность самостоятельно ходить были факторами, снижающим для них шанс тяжелого течения COVID-19.
По полученным прогностическим моделям, содержащим сведения о возрасте, поле, группе инвалидности, числе сопутствующих заболеваний и наличии или отсутствии ГБ, возможно предсказать вероятность развития пневмонии, а по сведениям о возрасте, поле, числе сопутствующих заболеваний, наличии или отсутствии ГБ и заболеваний почек – вероятность летального исхода у лиц, проживающих в ЗУДУ.


