Пандемия коронавирусной инфекции COVID-19 продолжает быстро развиваться. На момент начала нашего исследования (к 1 июля 2020 г.) в мире было зарегистрировано 10,4 млн случаев COVID-19, в том числе более 508 000 больных умерли [1]. Через год, к 29 июня 2021 г., было зарегистрировано более 180,5 млн случаев COVID-19 и 3 916 771 летальных исходов [2] .
Развитие новой пандемии происходит на фоне относительно старой, но не прекращающейся более 40 лет пандемии инфекции, вызываемой вирусом иммунодефицита человека (ВИЧ-инфекция, ВИЧ/СПИД). По оценкам ЮНЭЙДС, ВИЧ заразились 77,5 млн чел., из которых к концу 2020 г. 34,7 млн умерли от заболеваний, связанных с ВИЧ/СПИДом. К концу 2020 г. в мире жили с ВИЧ 37,6 (30,2–45,0) млн чел. В 2020 г. 1,5 млн чел. были инфицированы ВИЧ, и 690 000 чел. умерли от сопутствующих СПИДу заболеваний [3].
Несмотря на отличающиеся пути передачи этих инфекций, пожизненный характер заболевания ВИЧ-инфекцией обусловливает возможность заражения одного человека обоими вирусами, а характерный для ВИЧ-инфекции иммунодефицит предполагает более тяжелые проявления сочетанной болезни. Существует и определенное сходство этих заболеваний в связи с сопутствующими им стигмой и дискриминацией, а также социально-экономической значимостью указанных пандемий. Одновременное развитие пандемий неизбежно вызывает их негативное взаимодействие на уровне социального ответа на их распространение, в том числе на его финансово-экономическую составляющую.
Во многих странах мира, имеющих наибольшее число больных ВИЧ-инфекцией, одновременно регистрируется и высокое количество больных коронавирусной инфекцией COVID-19. Однако прямая корреляция между пораженностью населения ВИЧ-инфекцией и распространением коронавирусной инфекции отсутствует. Регистрация значительного числа случаев COVID-19 отмечается в регионах, характеризующихся высокой урбанизацией, имеющих значительный потенциал тестирования на эту новую инфекцию и оказания медицинской помощи больным.
На момент начала исследования, исходя из опыта эпидемий, вызванных вариантами вируса гриппа, предполагалось, что людям, живущим с ВИЧ (ЛЖВ), угрожает более тяжелое течение коронавирусной инфекции. В настоящее время продолжается изучение влияния коинфекции ВИЧ/COVID-19 на ЛЖВ. Ряд случаев инфицирования COVID-19 на фоне ВИЧ-инфекции был описан в публикациях из Китая, Испании, Германии, Италии, Великобритании и США [4–8]. До настоящего времени не было получено четких доказательств более высокого риска заболевания COVID-19 или особенного течения заболевания у ЛЖВ по сравнению с ВИЧ-негативными лицами. Более того, исследования, проведенные на когортах больных, получавших стационарную медицинскую помощь или обращавшихся за медицинской помощью в клинику, свидетельствовали о том, что коинфекция ВИЧ/COVID-19 не оказывает значительного влияния на течение заболевания, лечение или исходы коронавирусной инфекции. В ряде таких исследований ЛЖВ составляли около 1% [9, 10] Однако авторы одного из подобных исследований, проведенных в Испании, предположили, что стандартизированный уровень заболеваемости COVID-19 среди ЛЖВ был значительно (на 67%) ниже, чем среди населения в целом [11].
Важно заметить, что все вышеуказанные исследования изучали ЛЖВ с симптомами коронавирусной инфекции, госпитализированных или обратившихся в клиники, в то время как бессимптомная инфекция COVID-19 является весьма распространенным явлением [12]. Нам было неизвестно к началу исследования, насколько ЛЖВ склонны обращаться за медицинской помощью в клиники, особенно в условиях предупреждений быть особенно осторожными и строго придерживаться рекомендаций ВОЗ и ЮНЭЙДС в отношении COVID-19. Неизвестно, какая доля инфицированных ВИЧ имела легкое течение коронавирусной инфекции. Во время вспышек SARS и MERS было всего несколько сообщений о случаях легкого течения заболевания среди ЛЖВ.
Имеющиеся данные указывают на то, что риск тяжелого течения COVID-19 возрастает в зависимости от возраста, пола и некоторых хронических болезней, таких как сердечно-сосудистые заболевания, хронические заболевания легких, ожирение, онкологические заболевания и диабет. В исследовании, проведенном в США [13], было показано, что пациенты с недавним диагнозом расстройств, связанных с употреблением психоактивных веществ, имели существенно более высокий риск развития COVID-19, который был в 10 раз выше для людей, употребляющих опиоиды (ОШ = 10,244).
В одной из публикаций, основанной на мета-анализе (с использованием баз данных PubMed, Scopus, OVID, Web of Science и Cochrane Library, включая любые статьи, опбликованные в период с 1 января по 15 июня 2020 г.), сообщается, что распространенность ВИЧ-инфекции среди пациентов, госпитализированных с COVID-19, по-видимому, выше по сравнению с населением в целом, что свидетельствует о повышенной восприимчивости ЛЖВ к COVID-19. Суммарная распространенность ВИЧ среди пациентов с COVID- 19 составила 1,22% (95% ДИ 0,61–2,43%), что вдвое превышает распространенность среди населения в целом – 0,65% (95% ДИ 0,48–0,89%) [14].
Даже если ЛЖВ без иммунодефицита, получающие АРТ и имеющие подавленную вирусную нагрузку (ВН), не подвергаются повышенному риску тяжелого заболевания COVID-19, многие люди с ВИЧ имеют сопутствующие заболевания, которые относят их к группе риска по COVID-19. В частности, почти половина ЛЖВ в Европе старше 50 лет, а хронические проблемы со здоровьем, включая сердечно-сосудистые заболевания и хронические заболевания легких, встречаются у ЛЖВ чаще. Необходимо учитывать, что значительное число случаев коинфекции ВИЧ/COVID-19 регистрируется в более молодом возрасте, чем у ВИЧ-негативных госпитализированных пациентов с COVID-19.
В одной из немногочисленных публикаций по клиническому течению сочетанной инфекции ВИЧ/COVID- 19 в России было указано на высокую смертность от COVID-19, особенно в группе пациентов, не получавших АРТ: 7 случаев среди 29 пациентов, что составляет 24,1% [15].
Некоторое время велись дискуссии и исследования в отношении некоторых антиретровирусных препаратов (АРВП), которые теоретически могли иметь определенную активность в отношении COVID-19, однако достоверных данных об их эффективности в лечении COVID-19 получено не было [16]. При этом ряд стран в течение непродолжительного времени в 2020 г. использовали отдельные АРВП в стандартной терапии COVID-19.
ВОЗ и ЮНЭЙДС весной 2020 г. заявили о том, что пока не будет получено больше убедительной информации, ЛЖВ, особенно имеющие выраженный иммунодефицит или определяемую ВН, должны быть особенно осторожными и строго придерживаться рекомендаций по профилактике коронавируса. При этом было уделено особое внимание вопросам доступности лечения и услуг в связи с ВИЧ в условиях вспышки COVID-19, в частности, доступа к жизненно важной АРТ для ЛЖВ и к профилактике ВИЧ-инфекции для них и лиц, не инфицированных ВИЧ [17].
На момент разработки концепции исследования практически отсутствовала информация о распространенности COVID-19 среди ЛЖВ как в Российской Федерации, так и в мире, а также сведения о наличии или отсутствии влияния АРТ на COVID-19 среди этой категории. В связи с указанными пробелами в знаниях о коинфекции ВИЧ/COVID-19 и исключительной важностью получения бесперебойного лечения и медицинской помощи для ЛЖВ было проведено настоящее исследование. Оно проводилось совместно ФБУН «Центральный НИИ эпидемиологии» Роспотребнадзора (далее – ЦНИИЭ) и Коалицией по готовности к лечению (ITPCru) при поддержке ЮНЭЙДС.
Целью исследования было описание влияния эпидемии COVID-19 на оказание медицинской помощи при ВИЧ-инфекции и распространенности новой коронавирусной инфекции COVID-19 среди ЛЖВ.
Материалы и методы
Представлены результаты поперечного неинтервенционного эпидемиологического исследования с вторичным анализом эпидемиологической и клинической информации в отношении коинфекции ВИЧ/COVID-19. Сбор данных проводили путем анонимного анкетирования в сети Интернет. Данный метод был выбран как наиболее эффективный и безопасный, учитывая конфиденциальность информации, эпидемическую ситуацию по COVID-19 и необходимость получения данных от респондентов как обращающихся в медицинские организации, так и избегающих этого. Объектами исследования и дальнейшего анализа послужили данные интернет-опроса по структурированной анкете и полуструктурированного личного интервью с инфицированными ВИЧ респондентами, перенесшими COVID-19. Респондентам предлагалось самостоятельно заполнить структурированный опросник на интернет-сервисе для проведения опросов «Анкетолог». Готовность прохождения анкетирования необходимо было подтвердить информированным согласием.
При получении сведений о выявлении у респондентов-ЛЖВ коронавирусной инфекции COVID-19 участники исследования автоматически получали просьбу связаться с консультантом для уточнения необходимой эпидемиологической и клинической информации по случаю заболевания. Полуструктурированные интервью с респондентами для сбора эпидемиологической и клинической информации по случаю заболевания проводили анонимно по телефону/WhatsApp врач-инфекционист или равный консультант по выбору респондента.
Информация о проведении исследования для привлечения респондентов распространялась на сайтах Коалиции по готовности к лечению (ITPCru), Роспотребнадзора, Федерального научно-методического центра по профилактике и борьбе со СПИДом ЦНИИЭ, в социальных сетях и была опубликована в прессе (более 40 публикаций в СМИ).
В исследовании принял участие 931 респондент из 68 регионов России. Объектом исследования послужили ответы 852 лиц: 590 ВИЧ-позитивных (1-я группа) и 262 ВИЧ-негативных (2-я группа) респондентов, полученные в результате интернет-опроса по структурированной анкете на ресурсе «Анкетолог». Анкеты 79 респондентов, не имевших опыта тестирования на ВИЧ, согласно критериям исключения, не были включены в анализ.
Для анализа данных были использованы стандартные статистические пакеты программ SPSS, Excel.
Результаты
Половозрастное распределение в группах несколько отличалось: во 2-й группе женщины составили 77,1%, в 1-й – 62,4%. Остальные респонденты в обеих группах назвали себя мужчинами. В противоположность опрошенным, в популяции ЛЖВ в России большинство составляли мужчины (62,6%). Возрастное распределение опрошенных в целом соответствовало аналогичному в группах. В 1-й группе в возрасте 35–39 лет было 29,8% респондентов, 40–44 года – 23,2%, 30–34 года – 22,4%. Лица в возрасте 30–49 лет составили 86,3% всех инфицированных ВИЧ респондентов. Во 2-й группе наблюдалось более плавное распределение по возрасту согласно структуре популяции: 43,1% составили респонденты в возрасте от 30 до 44 лет, на молодежь в возрасте 18–24 лет приходилось 13,0%. Медиана возраста респондентов составила 38 (18– 67) лет. В анкетировании приняли участие жители 68 регионов России, в 4 анкетах были указаны другие страны (Таджикистан, Казахстан, Беларусь), однако респонденты указали, что проживают в Российской Федерации. Подавляющее большинство проживали в столичных городах наиболее пораженных ВИЧ-инфекцией субъектов Российской Федерации. 54,9% респондентов проживали в Москве, Санкт-Петербурге, Новосибирской, Московской, Самарской, Свердловской областях и Республике Бурятия.
В 1-й группе 98,6% респондентов сообщили, что состоят под диспансерным наблюдением в центре СПИДа или другой специализированной на ВИЧ/СПИД медицинской организации, 1,2% не состояли под наблюдением и 0,2% затруднились ответить.
562 (95,3%) опрошенных ЛЖВ получали АРТ, что существенно превышало среднероссийский охват лечением: по данным Росстата, в 2020 г. в России получали АРТ 83,6% от числа состоявших под диспансерным наблюдением1. Безусловно, охват лечением всех ЛЖВ был существенно ниже.
366 (65,1%) респондентов 1-й группы начали получать АРТ в течение последних 5 лет, в том числе 17,6% получали ее менее года, 47,5% – от 1 года до 5 лет, 23,8% – 5–10 лет, 10,7% – более 10 лет; 0,4% респондентов затруднились с ответом. Преимущественно ЛЖВ указывали на начало АРТ в 2019 (16,6%), 2018 (16,6%) и 2017 (10,7%) гг.
Среди опрошенных ЛЖВ 94,6% проходили исследование на иммунный статус (количество CD4-лимфоцитов) в течение последнего года: 34,9% – в течение последних 3 мес., 38,0% – от 3 до 6 мес. назад, и 21,7% – от 6 мес. до 1 года назад.
Подавляющее большинство респондентов не имели выраженного иммунодефицита в связи как с высоким охватом АРТ, так и с недавним установлением диагноза ВИЧ-инфекции. Согласно результатам последнего исследования на иммунный статус, у 57,6% ЛЖВ количество CD4+-лимфоцитов было > 500 клеток/ мкл, у 6,9% – 350–500 клеток/мкл, у 13,2% – < 350 клеток/ мкл.
Охват обследованием на ВН ВИЧ был тоже достаточно высок: 93,9% проходили это исследование в течение последнего года, в том числе 36,8% – в течение последних 3 мес., 33,7% – от 3 до 6 мес. назад, 23,4% – от 6 мес. до 1 года назад. Среди респондентов, указавших значения ВН, у 93,2% она составила < 1000 копий/мл, то есть фактически была подавлена. Однако обращает на себя внимание тот факт, что более 1/3 участников опроса затруднились указать свой уровень ВН, что довольно странно, учитывая высокую долю респондентов, получающих лечение. Можно предположить, что пациентам по каким-то причинам не были сообщены результаты исследования на ВН, или они не считали этот показатель важным, поэтому не запоминали его значение. Нельзя исключить, что в 2020 г. исследование проводилось далеко не сразу после забора образца. Если пересчитать долю респондентов ЛЖВ, указавших ВН < 1000 копий/мл среди лиц с известной ВН, то фактически лишь у 61,1% она была подавлена.
Среди респондентов 1-й группы, получающих АРТ, 43,1% принимали схемы, включающие ННИОТ, 26,6% – ИП и только 30,3% – ИИ. По данным респондентов, они чаще всего принимали ламивудин/тенофовир/эфавиренз (13,7% ответов), ламивудин/тенофовир/долутегравир (11,0%) и рилпивирин/тенофовир/эмтрицитабин (9,1%). Третьим препаратом в схеме наиболее часто являлись долутегравир (23,5%), эфавиренз (19,0%), лопинавир/ритонавир (13,3%), рилпивирин (9,1%), атазанавир (6,0%). Чаще всего в качестве нуклеозидной основы схемы АРТ использовались тенофовир (75%), абакавир (в 20%), зидовудин (5%). 41 (7,3%) респондент затруднился назвать препараты, которые принимает, что может вызывать серьезную обеспокоенность.
Отмечали на собственном опыте изменения в связи с пандемией COVID-19, которые негативно отразились на работе центра СПИДа (сокращение часов работы; уменьшение количества персонала, например, за счет перевода на лечение больных COVID-19 и т. п.), 34,3% респондентов, 61,2% не почувствовали изменений, 4,4% затруднились с ответом.
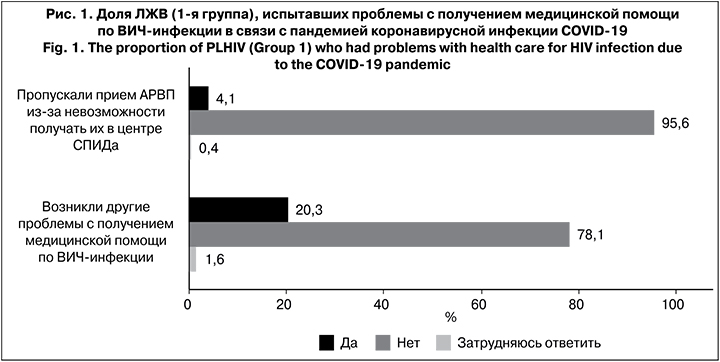
При этом в 1-й группе среди лиц, получающих АРТ, только 4,1% сообщили, что пропускали прием АРВП из-за невозможности получить их в центре СПИДа. У 20,3% респондентов возникли какие-либо другие проблемы с получением медицинской помощи по ВИЧ-инфекции в связи с пандемией коронавирусной инфекции COVID-19 (рис. 1). Среди респондентов 1-й группы, получающих АРТ, 70,5% сообщили, что не испытывали проблем с получением АРВП (табл. 1). Наиболее распространенными проблемами при получении АРВП во время эпидемии COVID-19 респонденты называли необходимость добираться на транспорте из-за большого расстояния (14,9% ответов) и страх заразиться коронавирусом при выходе из дома (10,0%). Лишь 3,7% ЛЖВ ответили, что центр СПИДа, который они обычно посещают, был закрыт либо работал в укороченном режиме, а 4,6% сообщили, что нужных лекарств не было в аптеке.

На момент исследования не было на руках АРВП у 0,5% респондентов, а 13,5% имели запас препаратов менее чем на 1 мес. 56,8% пациентов имели на руках АРВП на 2–3 мес. приема, 22,8% – на 1 мес., 6,4% – на 6 мес. При этом 22,6% респондентов сообщили, что АРВП им на дом доставляли сотрудники центра СПИДа (14,8%) или аутрич-работники (7,8%), а 71,7% получали АРВП как обычно (табл. 2). 26,7% респондентов сообщили, что изменились сроки, на которые выдаются АРВП в центре СПИДа во время пандемии.
Анкета содержала несколько вопросов о получения профилактических услуг по ВИЧ-инфекции. В частности, вопросы о доконтактной профилактике (ДКП) задавались ВИЧ-негативным респондентам и людям, не указавшим на опыт тестирования на ВИЧ. О получении в 2020 г. АРВП для профилактики ВИЧ сообщили лишь 2 (0,8%) респондента 2-й группы: эти люди указали, что не испытывали никаких проблем в получении АРВП. Еще 2 респондента этой группы затруднились ответить на вопрос о ДКП, но при этом сообщили, что у них возникли проблемы с получением препаратов для ДКП в условиях пандемии COVID-19, такие как страх заразиться коронавирусом при выходе из дома и карантин, который не позволял никуда пойти. Весьма необычно, что среди 76 респондентов, которые ответили, что никогда не проходили тестирование на ВИЧ, 6 (7,9%) чел. сообщили о получении в 2020 г. АРВП для ДКП ВИЧ, из них 5 чел. не испытывали никаких проблем в получении таких препаратов. Возможно, они не знали о том, что проходили тестирование на ВИЧ.
К другим проблемам с получением профилактических услуг по ВИЧ-инфекции в условиях пандемии COVID-19 респонденты относили невозможность получить презервативы или средства для снижения вреда, а также отсутствие информации о том, куда идти, чтобы получить средства профилактики в условиях карантина. Эти проблемы называли преимущественно респонденты 1-й группы. Подавляющее большинство респондентов 2-й группы и не проходивших тестирование на ВИЧ респондентов (69,5 и 63,2% соответственно) указали, что не пользуются услугами профилактики ВИЧ-инфекции, а 21,4 и 23,7% соответственно не испытывали никаких проблем в получении профилактических услуг.
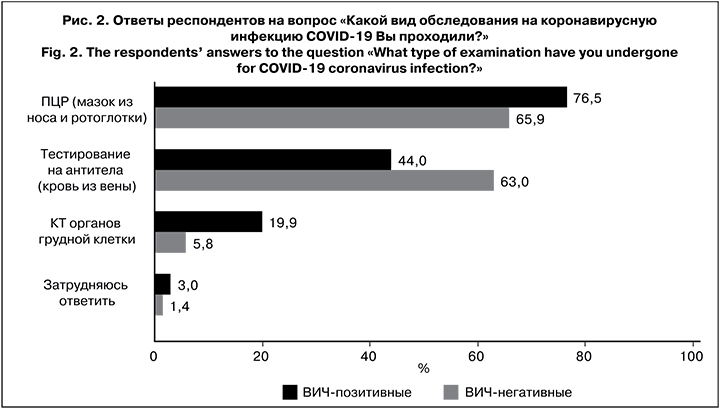
Доля прошедших обследование на COVID-19 и обратившихся за медицинской помощью в связи с этим заболеванием в группах существенно различалась. Во 2-й группе обследование на COVID-19 проходили 52,7% респондентов (95% ДИ 46,6–58,9%), в 1-й группе 28,1% (95% ДИ 24,6–31,7%) сообщили, что проходили обследование на коронавирусную инфекцию. Как видно по диапазонам ДИ, различия между группами были достоверны. Во 2-й группе был выявлен достоверно более высокий охват обследованием на коронавирусную инфекцию COVID-19 по сравнению с 1-й группой (ОШ = 2,82; р < 0,05).
Можно предположить, что в качестве ВИЧ-негативных участников в исследовании с более высокой вероятностью могли принять участие медицинские работники и волонтеры, которые получали рассылку с новостями о проведении исследования и с более высокой вероятностью могли быть посетителями информационных ресурсов, на которых размещалась информация об исследовании. Возможно, этим можно объяснить тот факт, что респонденты 2-й группы проходили обследование на коронавирусную инфекцию COVID-19 или обращались к врачу в связи с ее симптомами почти в 2 раза чаще. Другим объяснением может быть нежелание ЛЖВ обращаться в медицинские организации за любой помощью, включая обследование, в связи с предупреждениями быть особенно осторожными и строго придерживаться рекомендаций ВОЗ и ЮНЭЙДС в отношении COVID-19.
Различались и виды исследований на коронавирусную инфекцию COVID-19, проведенные в группах (рис. 2). В 1-й группе это была преимущественно ПЦР (мазок из носа и ротоглотки) – 76,5%, а во 2-й – тестирование на антитела (63,0%). Существенно большая доля респондентов 1-й группы проходила КТ органов грудной клетки (19,9% против 5,8% во 2-й группе). Вероятно, это было связано с наличием у них симптомов COVID-19.
О наличии каких-либо симптомов, характерных для COVID-19, в период с марта 2020 г. в 1-й группе сообщили 55,3%, во 2-й – 35,1%. Респонденты 1-й группы гораздо чаще отмечали все перечисленные симптомы, в том числе кашель (22,5%), повышение температуры тела (21,4%), усталость (38,0%), головную боль (27,5%), заложенность носа или насморк (25,9%), боль в мышцах или суставах (20,7%), одышку (17,3%), боль в горле и диарею (17,8%), боль в груди (14,6%), потерю обоняния и/или вкуса (9,8%). У большинства одновременно отмечалось несколько симптомов, часто встречающихся при COVID-19. Частота встречаемости различных симптомов во 2-й группе была в среднем в 2 раза ниже: усталость ощущали 22,9%, головную боль – 18,3%, заложенность носа или насморк – 13,7%, боль в горле – 12,6%, кашель – 10,3%, боль в мышцах или суставах – 8,8%, повышенную температуру тела – 8,0%, диарею – 6,9%, одышку – 6,1%, боль в груди – 5,3%, потерю обоняния и/или вкуса – 4,6%.
Частота сопутствующих заболеваний, которые могли осложнить течение коронавирусной инфекции COVID-19, в обеих группах отличалась несущественно. Однако в 1-й группе туберкулез встречался в 9 раз чаще, вирусные гепатиты/болезни печени – в 5 раз, заболевания почек, легких, ЖКТ – в 3–4 раза.
 По данным исследования, в 1-й группе маркеры коронавирусной инфекции COVID-19 выявляли достоверно чаще – у 23,5% респондентов (ОШ = 4,70; р < 0,05) (рис. 3). Во 2-й группе 6,5% респондентов оказались позитивными к COVID-19.
По данным исследования, в 1-й группе маркеры коронавирусной инфекции COVID-19 выявляли достоверно чаще – у 23,5% респондентов (ОШ = 4,70; р < 0,05) (рис. 3). Во 2-й группе 6,5% респондентов оказались позитивными к COVID-19.
Еще более значительные различия между группами были выявлены по числу респондентов, которым был поставлен диагноз коронавирусной инфекции COVID- 19. Среди 590 респондентов 1-й группы диагноз коронавирусной инфекции COVID-19 был поставлен 29 (17,5% от обследованных на COVID-19 и 4,9% среди всех опрошенных ЛЖВ). Диагноз чаще устанавливали в 1-й группе, чем во 2-й (ОШ = 7,30; р < 0,05), где он был поставлен 4 респондентам (2,9% от обследованных на COVID-19 и 1,5% среди всех опрошенных ВИЧ-негативных).
Только 41,4% ЛЖВ сообщили о заболевании COVID- 19 в центр СПИДа. Этот факт может объяснять наличие у специалистов российских центров СПИДа на момент проведения исследования устойчивого мнения о том, что среди пациентов с ВИЧ-инфекцией COVID- 19 встречается довольно редко.
57,2% опрошенных были лично знакомы с людьми, которым был поставлен диагноз коронавирусной инфекции COVID-19. При этом во 2-й группе по сравнению с 1-й существенно больше респондентов имели больных коронавирусной инфекцией COVID- 19 в близком окружении (73,7 и 49,8% соответственно). В 1-й группе 14,9% респондентов сообщили, что лично знали инфицированных ВИЧ, больных или переболевших COVID-19; во 2-й группе таких было 8,0%.
Личный риск заразиться коронавирусной инфекцией COVID-19 респонденты оценивали в основном как умеренный – в среднем 5 баллов по 10-балльной шкале. Респонденты в обеих группах преимущественно полагали, что такой риск связан с пользованием общественным транспортом и контактами с большим количеством людей после начала пандемии. 70,2% респондентов 2-й группы при этом считали, что у них не было риска заразиться, поскольку они постоянно использовали маску, перчатки и другие меры предосторожности, или находились на самоизоляции; в 1-й группе такие ответы дали 60,2%. Не верили в коронавирусную инфекцию в 1-й группе 10,3% респондентов, во 2-й – 3,8%.
Подгруппа респондентов ЛЖВ, имеющих диагноз или позитивные результаты тестирования на COVID- 19 (39 чел.), имела существенные отличия от 1-й группы в целом. Среди ЛЖВ, перенесших коронавирусную инфекцию COVID-19, было существенно больше мужчин (51,3%) и лиц с иммунодефицитом. У 20,6% количество СD4+-лимфоцитов было < 350 клеток/мкл, только у 56,4% отмечалось относительно благополучное состояние иммунной системы. В противоположность всей выборке ЛЖВ, 56,4% респондентов ЛЖВ, перенесших COVID-19, принимали АРТ более 5 лет, стаж приема АРТ менее 1 года имели только 12,8%, от 1 года до 5 лет – 25,6%.
Согласно полуструктурированному интервью 24 ЛЖВ, имеющих диагноз или лабораторные маркеры COVID-19, медиана продолжительности жизни с ВИЧ у перенесших COVID-19 составила 10,5 лет. Медиана продолжительности заболевания COVID- 19 в 1-й группе в целом составила 17,5 дня. О бессимптомном течении заболевания заявили только 2,6% перенесших COVID-19. Легкое течение инфекции отмечено у 34,8% респондентов, средней тяжести – у 65,2%, случаев тяжелого течения не зафиксировано. В большинстве случаев респонденты сообщили о полисимптоматике, только у 8,3% выявлены моносимптомы: потеря обоняния/вкуса и боль в грудной клетке. Среди всего спектра симптомов преобладали повышение температуры (75,0%), усталость (70,8%), потеря обоняния или/и вкуса (66,6%), кашель (58,3%), одышка (54,2%), головная боль (54,2%), боль в мышцах (41,7%). У 41,7% опрошенных была диагностирована пневмония. Госпитализированы 37,5% респондентов, среди них в реанимацию/ОИТ никого не переводили. 20,8% респондентов не обращались за медицинской помощью в связи с COVID-19. В 1-й группе у 87,5% участников исследования имелись сопутствующие заболевания. При лечении COVID-19 у них часто использовали антибактериальные препараты (66,7%), отхаркивающие и бронхолитики (25,0%). Восстановившимися после перенесенного COVID-19 считали себя 37,5% респондентов, остальные испытывали проблемы со здоровьем: слабость, кашель, снижение толерантности к физическим нагрузкам, «ломота в теле».
Обсуждение
Недостатком, снижающим достоверность полученных данных, является смещение выборки. Большинство респондентов во всех группах составили женщины. Выборка среди инфицированных ВИЧ была смещена в сторону лиц, приверженных диспансерному наблюдению и лечению, что связано с первым фактом. Кроме того, в исследовании с большей вероятностью могли не принять участие респонденты, которые пока не столкнулись с COVID-19 лично.
Заключение
Исследование показало негативное влияние пандемии коронавирусной инфекции COVID-19 на оказание медицинской помощи при ВИЧ-инфекции в Российской Федерации. Треть респондентов, назвавших себя ЛЖВ, отмечали на собственном опыте изменения в связи с пандемией COVID-19, которые негативно отразились на работе центра СПИДа, а 4,1% респондентов пропускали прием АРВП из-за невозможности получить их в центре СПИДа. Большинство респондентов, назвавших себя ЛЖВ, сообщили, что не испытывали проблем с получением АРВП; 22,6% респондентов препараты доставлялись на дом.
Согласно полученным данным, среди участников исследования люди, назвавшие себя инфицированными ВИЧ, вероятно, были более подвержены коронавирусной инфекции COVID-19 по сравнению с респондентами, назвавшими себя ВИЧ-негативными.
При наличии симптомов, характерных для COVID- 19, ЛЖВ в 2 раза реже, чем ВИЧ-негативные респонденты, проходили обследование на коронавирусную инфекцию и реже обращались за медицинской помощью.
У респондентов, назвавших себя ЛЖВ, значительно чаще встречались сопутствующие заболевания (туберкулез, вирусные гепатиты, заболевания печени, почек, легких, ЖКТ), которые могли не только осложнить течение коронавирусной инфекции COVID-19, но и вызвать существенные сложности при диагностике заболевания.
Среди респондентов, назвавших себя ЛЖВ и сообщивших о перенесенном COVID-19, большинство составляли мужчины со стажем жизни с ВИЧ более 10 лет. 94,9% из них принимали АРТ и, согласно ответам, большинство не имели выраженного иммунодефицита и определяемой ВН. Однако в 1-й группе респондентов, сообщивших о перенесенном COVID- 19, было больше лиц с тяжелым иммунодефицитом (< 200 клеток/мкл), а 41,0% из них затруднились ответить на вопрос о последнем значении ВН.
У большинства респондентов, сообщивших о ВИЧ и COVID-19, имелся объективный риск заражения COVID-19 в связи с наличием значительного количества источников инфекции в близком окружении и низким уровнем использования средств индивидуальной защиты, а также недооценкой реального личного риска инфицирования COVID-19.
Вероятно, необходимо рекомендовать повышенные меры предосторожности в связи с COVID-19 для ЛЖВ, включая профилактические мероприятия, вакцинацию, раннюю диагностику и лечение COVID-19.
Учитывая подъем заболеваемости COVID-19, необходимо вести дальнейшее изучение повышенной уязвимости в отношении COVID-19 для ЛЖВ, включая углубленные исследования ее причин среди пациентов с ВИЧ. С целью повышения достоверности данных необходимо принять дополнительные меры по соблюдению репрезентативности выборки.