Несмотря на то что антибиотики не входят в Перечень лекарственных средств, отпускаемых без рецепта врача, их продажа свободно осуществляется во всех аптечных учреждениях нашей страны, что в конечном итоге составляет серьезнейшую проблему, связанную с высокой частотой их нерационального применения, в первую очередь, при инфекциях дыхательных путей. Так, по данным фармакоэпидемиологических исследований [1], порядка 60% населения нашей страны применяют антибиотики при наличии симптомов вирусной инфекции, причем в числе наиболее популярных препаратов фигурируют устаревшие, порой потенциально токсичные средства. Кроме того, многие авторы указывают и на врачебные ошибки при назначении антибиотиков в амбулаторной и стационарной практике [2].
Наиболее опасными резистентными микроорганизмами в настоящее время считаются экстремально- и панрезистентные штаммы Pseudomonas aeruginosa и Acinetobacter spp., штаммы представителей семейства Enterobacteriaceae, продуцирующие β-лактамазы расширенного спектра (ESBL) и карбапенемазы, метициллинорезистентный Staphylococcus aureus (MRSA), ванкомицинорезистентные энтерококки, а также Clostridium difficile [3, 4]. При этом, как указывают эксперты Американского общества по инфекционным болезням (Infectious Diseases Society of America – IDSA), для лечения серьезных жизнеугрожающих инфекций, вызываемых резистентными микроорганизмами, практически нет новых антимикробных средств [5].

В России использование в качестве ориентира для формирования стратегии антибактериальной терапии результатов многоцентровых исследований, охватывающих значительные регионы, может привести к определенным ошибкам. При всей важности результатов таких исследований приоритет должен сохраняться за более локальными данными, вероятно, в пределах регионов, характеризующихся устойчивыми внутренними экономическими и социальными связями [2]
Целью нашего исследования стал анализ чувствительности микрофлоры, выделенной при бактериологическом исследовании мазков из верхних дыхательных путей, к антибактериальным препаратам у пациентов с острыми респираторными заболеваниями (ОРЗ), потребовавшими их госпитализации в ГБУЗ «Центр по профилактике и борьбе со СПИДом и инфекционными заболеваниями» Министерства здравоохранения Кабардино-Балкарской Республики (Нальчик).
Материалы и методы
В эпидемический сезон подъема заболеваемости ОРЗ с октября 2015 г. по апрель 2016 г. было получено 935 высевов у детей и 312 высевов у взрослых. Использовали диско-диффузионный метод оценки чувствительности микроорганизмов к антимикробным препаратам, разработанный Европейским комитетом по определению чувствительности микроорганизмов к антибиотикам [European Committee on Antimicrobial Susceptibility Testing – EUCAST; http://www.eucast.org (версия 4.0, июнь 2014 г.)]. Использовали методику посева слизи из полости носа и зева и мокроты на микрофлору и чувствительность к антибиотикам. Анализу подвергалась антибиотикограмма, результаты которой оценивали по уровню резистентности микроорганизмов к разным антибактериальным препаратам.

Результаты и обсуждение
Чаще всего в мазках из верхних дыхательных путей высевали S. aureus и S. epidermitidis – у 458 детей и 168 взрослых. Наибольшая чувствительность определялась к гентамицину, цефалоспоринам 1–4-го поколения, рифампицину и доксициклину. Менее чувствительны стафилококки оказались к ципрофлоксацину и оксациллину. Резистентность к ванкомицину составила более 20% (особенно у детей) и к 14-, 15-членным макролидам (эритромицину, азитромицину). При лечении ОРЗ стоит отказаться от применения ко-тримоксазола: согласно нашим данным, резистентность S. aureus и S. epidermitidis к нему у детей составляет 75%, у взрослых – 67,2%, что значительно отличается от результатов, полученных в многоцентровых исследованиях [6, 7] (рис. 1).
Второе место по частоте высеваемости из верхних дыхательных путей занимает Streptococcus spp. – он обнаружен у 277 детей и у 172 взрослых. Самая низкая чувствительность стрептококков определена к оксациллину, азитромицину и цефалоспоринам 2–4-го поколения, причем значительно более выражена она у детей (табл. 1).
Отдельно была проанализирована чувствительность к антибиотикам Streptococcus pneumoniae у 98 взрослых и детей. В отличие от S. aureus, у Str. pneumoniae сохранена чувствительность к азитромицину, цефалоспоринам 1–4-го поколения, эритромицину и ванкомицину (число резистентных штаммов не превышало 10%). Была отмечена высокая (более 25%) резистентность к оксациллину и ко-тримоксазолу.
Интересные данные получены при определении резистентности Str. pyogenes у 41 ребенка с клиническими проявлениями скарлатины (рис. 2). Согласно результатам исследования, при лечении скарлатины имеет смысл отказаться от применения эритромицина (резистентность к нему Str. pyogenes – 38,7%), азитромицина (48,6%) и оксациллина (54,3%).
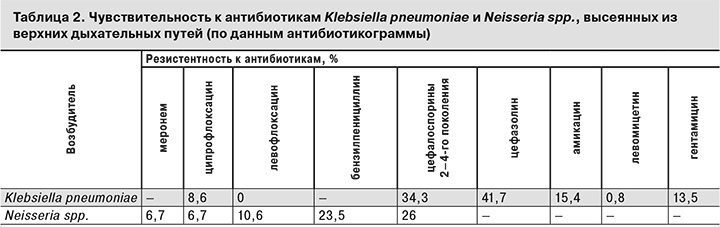
Ожидаемо неутешительные результаты были получены при анализе чувствительности к антибиотикам Klebsiella pneumoniaе, выделенной у 39 детей и взрослых. Этот возбудитель сохраняет полную чувствительность к фторхинолонам 2-го поколения, в то же время резистентность к ципрофлоксацину составляет уже 10%, а к цефалоспоринам – до 40%. Такие же настораживающие результаты были получены при анализе чувствительности к антибиотикам Neisseria spp., выделенной из верхних дыхательных путей у 60 детей и взрослых. Оказалось, что наименее чувствителен этот возбудитель к бензилпенициллину и цефалоспоринам 2–4-го поколения (резистентность – 23 и 26% соответственно), что, возможно, требует пересмотра эмпирической терапии при подозрении на менингококковую инфекцию (табл. 2).
Таким образом, можно говорить о более выраженной резистентности к антимикробным препаратам у детей по сравнению со взрослыми, что, по-видимому, связано с нерациональным этиотропным лечением детей на амбулаторном этапе и распространенным самолечением [8].
Настораживает высокая (более 27%) резистентность St. aureus к ванкомицину у детей, что представляет значительные проблемы при проведении этиотропной терапии, и не только ОРЗ.
И, наконец, при лечении скарлатины стоит отказаться от применения эритромицина, азитромицина и оксациллина в связи с резистентностью возбудителя к этим препаратам больше 40%.
Необходимо подчеркнуть, что разработка новых антимикробных препаратов является не единственным способом борьбы с инфекционными заболеваниями. Анализ математической модели, в которой скорость разработки новых антибиотиков была сопоставлена со скоростью их устаревания за счет формирования микробной устойчивости, показал, что в долгосрочной перспективе работа над замедлением эволюции бактерий для борьбы с инфекциями эффективнее, чем создание новых антибиотиков [9]. Возможно, в будущем разработка таких методов станет основным направлением развития антимикробной терапии.