Новая коронавирусная инфекция (COVID-19), начавшаяся в декабре 2019 г. в г. Ухань Китайской Народной Республики, за несколько месяцев распространилась практически по всему миру, став пандемией. Новое заболевание характеризовалось высокой скоростью распространения, обусловленной воздушно-капельным путем передачи возбудителя, длительным инкубационным периодом, высокой плотностью населения в агломерациях и его высокой мобильностью в эпицентрах инфекции. По официальным данным, на 01.10.2021 г. уже зарегистрировано практически 240 млн случаев инфицирования COVID-19 и около 5 млн летальных исходов [1–4].
Появление нового возбудителя и новой инфекции поставило перед специалистами здравоохранения задачи быстрой диагностики и экстренного оказания высокоспециализированной медицинской помощи заболевшим. На всех этапах пандемии во всех странах мира велись интенсивное изучение клинических и эпидемиологических особенностей этого заболевания и разработка новых средств его профилактики и лечения [5–11].
В условиях пандемии COVID-19 особую актуальность приобрели исследования, связанные с оценкой частоты встречаемости и клинической значимости отдельных проявлений заболевания, а также анализ последствий перенесенной инфекции в ближайшей и отдаленной перспективе, что необходимо для своевременной диагностики и лечения этой инфекции и проведения коррекционных мероприятий в программах реабилитации пострадавших в раннем и позднем восстановительном периоде.
Цель исследования – анализ клинических проявлений новой коронавирусной инфекции у медицинских работников и оценка ее последствий для здоровья в ближайшей и отдаленной перспективе.
Материалы и методы
Для анализа особенностей клинических проявлений COVID-19 у сотрудников медицинских организаций использована разработанная авторами онлайн-анкета, включавшая 66 вопросов, объединенных в несколько блоков: паспортную часть, эпидемиологический анамнез, характеристику клинических проявлений болезни, обследования и лечения, а также ответы на вопросы по оценке последствий перенесенного заболевания.
Анкета была создана на базе электронных сервисов Google (доступна по ссылке: https://docs.google.com/forms/d/1Fs-utZ5WbVfJjFinG5-bednx43JejAja9 PWfVTFumDY/edit) и распространялась среди сотрудников медицинских организаций (МО) посредством корпоративной электронной почты или мессенджера WhatsApp. В исследовании участвовали 238 сотрудников МО, которые переболели коронавирусной инфекцией в 2020 г.
Применяли эпидемиологический (описательно-оценочный и аналитический), социологический и статистический методы исследования. При анализе полученных данных использовали общепринятые статистические приемы. Для сравнения вероятности исхода (развития более тяжелых форм коронавирусной инфекции) в зависимости от воздействия различных факторов риска составляли четырехпольную таблицу сопряженности и рассчитывали отношение шансов (OR). Статистическую значимость различий оценивали по критерию χ2. Различия считали достоверными при р < 0,05. Для статистической обработки материалов использовали электронные сервисы Google, пакет прикладных программ Microsoft Office 2013 и онлайн-сервис https://medstatistic.ru/.
Результаты
В опросе приняли участие сотрудники разных специальностей и должностей: врачи, средние и младшие медицинские работники, административно-управленческий персонал, а также работники технической и хозяйственной служб (табл. 1). Средний возраст переболевших COVID-19 составил 38,9 года. Среди респондентов было 84,5% женщины и 15,5% мужчин.
В так называемую первую волну пандемии (с апреля по август 2020 г.) коронавирусную инфекцию перенесли 27 (11,3%) сотрудников, а во вторую волну (с сентября по декабрь 2020 г.) – 211 (88,7%). Таким образом, у 170 (71,4%) чел. от начала заболевания прошло до 3 мес., у 23 (22,3%) – от 3 до 6 мес., у 15 (6,3%) – более 6 мес.
У 178 (74,8%) участников опроса заболевание протекало в форме острой респираторной инфекции легкой или средней степени тяжести, у 52 (21,8%) – в виде интерстициальной пневмонии и у 8 (3,4%) клинические проявления вообще отсутствовали.
Большинство сотрудников (216 или 90,8%) лечились дома, 22 (9,2%) потребовалось лечение в стационаре. У 82 (34,5%) заболевших были определены показания для проведения КТ-исследования легких и средостения. Среди них патологические изменения на КТ были выявлены у 63,4%. Чаще всего на томограмме наблюдали картину, соответствующую КТ-1 (у 41 чел. или 78,8%),только у 9 (17,3%) чел. она соответствовала 2-й и у 2 (3,8%) чел. – 3-й степени поражения.
Среди клинических проявлений COVID-19 наиболее часто беспокоили слабость – в 195 (81,9%) случаях, повышение температуры тела – в 183 (76,9%) и потеря обоняния (аносмия) – в 179 (75,2%). У 91 (49,7%) заболевшего температура тела поднималась до 37,5 0С, у 61 (33,3%) сотрудника она варьировала от 37,5 до 38,5 0С, а у 31 (16,9%) была выше 38,5 0С.
Помимо этого, многие заболевшие предъявляли жалобы на затруднение носового дыхания и серозно-слизистые выделения из носовых ходов (145 или 60,9%), боли в мышцах, суставах (130 или 54,6%), головную боль (127 или 53,4%), кашель (115 или 48,3%), преимущественно сухой (до 83,7%). Некоторые респонденты отмечали агевзию (112 или 47,1%), боль в горле (89 или 37,4%), боль в глазах (69 или 29,0%), головокружение (67 или 28,2%), чувство «сдавленности» в грудной клетке (67 или 28,2%), одышку (50 или 21,0%) и диспепсические проявления в виде тошноты или рвоты (24 или 10,1%). У 44 (18,5%) чел. был диарейный синдром. В единичных случаях сотрудники указывали на избыточную потливость, нарушение сердечного ритма, металлический привкус во рту, боль в эпигастральной области, высыпания на коже пупулезного или пятнисто-папулезного характера, нарушение сна, судороги в нижних конечностях. Указанные клинические проявления сохранялись у заболевших в интервале от 1 до 28 дней, в среднем 10,2 дня.
Для коронавирусной инфекции была характерна длительная персистенция возбудителя в организме. Установлено, что после исчезновения основных симптомов COVID-19 у большинство сотрудников при исследовании методом ПЦР в режиме реального времени продолжали выделять антиген вируса в мазках из зева и носа, что свидетельствовало об их эпидемиологической опасности как источников инфекции. Длительная персистенция вируса повлияла на продолжительность их нетрудоспособности. В результате средний период отсутствия на рабочем месте сотрудника с COVID-19 составлял 20,9 дня (от 13 до 45 дней). Помимо этого было отмечено, что при разных клинических формах COVID-19 период выделения вируса во внешнюю среду был различным. Так, у 8 чел. с бессимптомными формами коронавирусной инфекции средние сроки персистенции вируса составляли 18,7 дня (от 11 до 22 дней). У 178 чел. с проявлением COVID- 19 в виде острой респираторной инфекции средний период выделения вируса соответствовал 20,6 дня (от 13 до 34 дней). У 52 сотрудников, которые перенесли коронавирусную инфекцию в виде интерстициальной пневмонии, срок выделения вируса составлял 24,2 дня (от 14 до 45 дней), что следует учитывать при принятии решения о допуске переболевших сотрудников к работе в МО.
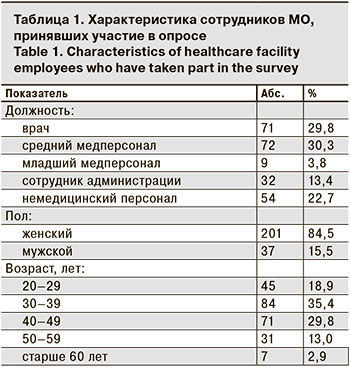
Была проведена оценка влияния сопутствующей патологии у медицинских работников на клинические проявления COVID-19, развитие более тяжелых форм заболевания. Установлено, что наличие такой фоновой патологии, как хронические заболевания дыхательной, сердечно-сосудистой, мочеполовой, нервной систем, желудочно-кишечного тракта, онкопатология, аллергические и аутоиммунные заболевания, сахарный диабет, герпесвирусная инфекция повышали риск развития более тяжелых форм коронавирусной инфекции – OR от 1,33 до 11,33 (табл. 2). Однако статистически значимые различия (p < 0,05) были получены только для хронических заболеваний мочеполовой системы и сахарного диабета. При других состояниях значимость различий не была подтверждена, что требует дополнительного изучения.
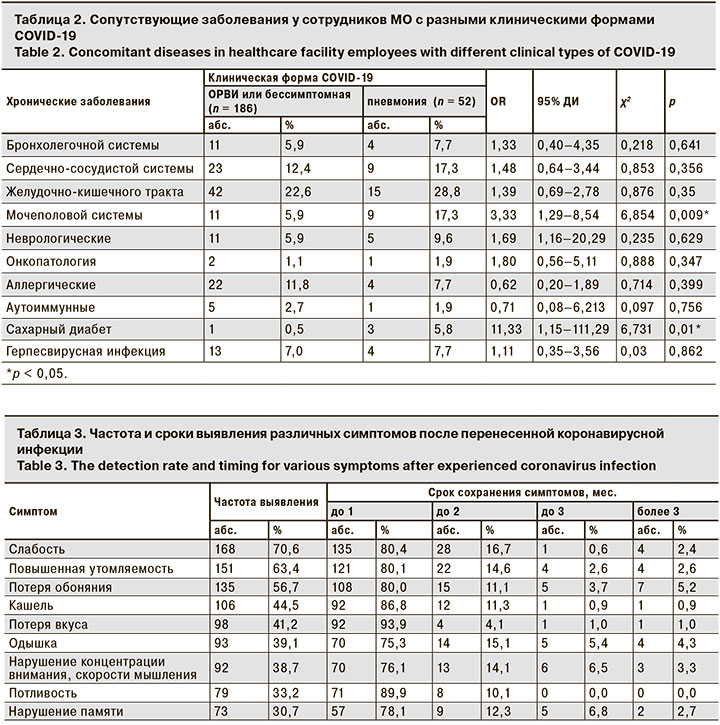
Многие респонденты отмечали, что после купирования основных проявлений COVID-19 некоторые симптомы сохранялись довольно долго, что было показанием для проведения реабилитационных мероприятий (табл. 3). Однако только 8 (3,3%) сотрудников после перенесенной коронавирусной инфекции прошли курс медицинской реабилитации (дыхательная гимнастика, гипокситерапия и лечебная физкультура).
Из клинических проявлений после перенесенного заболевания наиболее часто респонденты отмечали сохраняющуюся общую слабость и повышенную утомляемость (70,6 и 63,4% соответственно). В большинстве случаев эти симптомы продолжались не более 1 мес., хотя у части переболевших они сохранялись течение 3 и более мес. после COVID-19.
56,7% сотрудников жаловались на длительную аносмию, а у 5,2% этот симптом сохранялся более 3 мес.
У 106 (44,5%) переболевших оставался кашель, в том числе в 77,4% случаев это был непродуктивный кашель. 42 (50,0%) сотрудников указывали, что это был редкий кашель, однако 27 (32,1%) чел. отмечали, что в течение дня приступы кашля могли продолжаться до 15 мин., а у 15 (17,9%) чел. – даже в течение часа.
Среди респондентов 98 (41,2%) чел. отметили потерю вкусовых ощущений после исчезновения основных симптомов, в том числе у 93,9% эти проявления сохранялись в течение 1 мес., у 4,1% – 2 мес., у 1,0% – 3 мес. и у 1,0% – более 3 мес.
93 (39,1%) участники опроса указали на длительное сохранение одышки. При этом у 36,6% из них одышка появлялась только при интенсивной нагрузке, у 54,8% – при быстрой ходьбе или подъеме на небольшое возвышение. У 8,6% одышка была настолько выраженной, что требовала снижения двигательной активности или вообще ее прекращения.
Многие переболевшие отмечали нарушение некоторых когнитивных функций. Так, 92 (38,7%) чел. после заболевания отметили нарушение концентрации внимания, скорости мышления; 73 (30,7% – нарушение памяти. У 76,1–78,1% эти проявления сохранялись в течение первого мес. после заболевания, хотя у части сотрудников – в течение 3–5 мес.
79 (33,2%) участников исследования указали на повышенную потливость, которая сохранялась до 2 мес. после перенесенного заболевания.
Несколько реже после перенесенной коронавирусной инфекции сотрудники отмечали повышение температуры тела до 37,5 0С, особенно в вечернее время, головную боль, высыпания на коже, выпадение волос, боли в нижних конечностях и пояснице, нарушение сна, тревожность, повышение АД, чувство «сдавленности» в грудной клетке.
При оценке переносимости физических нагрузок после заболевания было установлено, что 136 (57,1%) сотрудников не чувствовали изменений и могли выдерживать такие же нагрузки, как и до заболевания. При этом 82 (34,5%) чел. отметили, что физические нагрузки после перенесенного COVID-19 им даются несколько тяжелее, 16 (6,7%) чел. – что нагрузки даются значительно тяжелее, а 4 (1,7%) чел. вообще отметили, что стали испытывать страх перед любыми физическими нагрузками и упражнениями.
При анализе переносимости умственных нагрузок было установлено, что 180 (75,6%) сотрудников не чувствуют никаких изменений. 46 (19,3%) чел. ответили, что умственные нагрузки им даются несколько тяжелее, чем ранее, и они медленнее решают поставленные задачи, быстро истощаются и не могут сосредоточиться, а 12 (5,0%) чел. указали, что интеллектуальные нагрузки им даются существенно тяжелее, а решение стандартных задач занимает гораздо больше времени, чем до болезни.
Также в анкетах были отмечены изменения психоэмоционального состояния переболевших коронавирусной инфекцией. Стабильное состояние без каких-либо изменений сохранили 172 (72,3%) сотрудника, 19 (8,0%) указали, что стали проще относиться к своим проблемам и сложным вопросам, а 39 (16,4%) после заболевания стали более тревожными, раздражительными, у них появились опасения за свое будущее. Еще 8 (3,1%) чел. после заболевания обратили внимание на частые перепады настроения, выраженное нарушение сна, более негативное отношение к людям и разным жизненным ситуациям.
Обсуждение
По различным аспектам клинических проявлений новой коронавирусной инфекции уже проведено достаточно много исследований и опубликовано большое количество работ [12–17]. Полученные в нашем исследовании данные в целом коррелируют с результатами других авторов [5–17]. При этом в настоящем исследовании сделан акцент на заболеваемость медицинского персонала, который является группой риска по заражению COVID-19, представлены основные характеристики заболеваемости коронавирусной инфекцией в этой профессиональной группе, а также получены актуальные данные о сроках персистенции вируса и периоде нетрудоспособности инфицированных сотрудников МО.
Необходимо отметить, что уже появились исследования, в которых проводилась оценка общего психоэмоционального состояния медицинских работников и распространенности среди них тревожности и депрессивных состояний, что имеет важное значение для разработки коррекционных мероприятий по созданию комфортной рабочей среды в МО [18–21].
Однако работ, посвященных изучению последствий перенесенного заболевания в ближайшей и отдаленной перспективе, пока довольно мало [22–26]. Эти единичные исследования посвящены оценке кардиологических, неврологических, психологических, психосоциальных последствий. В связи с этим полученные нами данные относительно последствий заболевания для общего состояния, физического и психоэмоционального здоровья медицинских работников представляют большой научный и практический интерес.
Заключение
В результате проведенного исследования получены данные об основных клинических проявлениях новой коронавирусной инфекции у медицинских работников, их выраженности и продолжительности, а также длительности персистенции вируса и последствиях перенесенного заболевания для здоровья переболевших, что может быть использовано при разработке программ реабилитации для лиц, перенесших COVID- 19 различной степени тяжести.