Акушерство занимает особое место в профилактике инфекций, связанных с оказанием медицинской помощи (ИСМП), как в историческом аспекте, так и на современном этапе развития здравоохранения. Послеродовые инфекционно-воспалительные заболевания родильниц представляют важную медико-социальную проблему и являются одной из основных причин материнской заболеваемости и смертности [1–3].
Современное акушерство, с одной стороны, ориентировано на естественное течение родового акта при минимальном вмешательстве медицинских работников в процесс родов, а с другой – сопряжено с высокой хирургической активностью. По данным ВОЗ, применение абдоминального родоразрешения приняло характер эпидемии, а операция кесарева сечения признана самой распространенной в мире. В России частота оперативных родоразрешений также из года в год увеличивается, составляя в ряде регионов до 30–35% [1, 4].
Абдоминальное родоразрешение и его роль в снижении материнской смертности и неблагоприятных перинатальных исходов – одна из самых обсуждаемых проблем как среди акушеров-гинекологов, так и среди эпидемиологов [1, 5].
Кесарево сечение, несмотря на совершенствование техники операции, использование современных шовных материалов и периоперационной антибиотикопрофилактики, остается фактором риска возникновения послеродовых инфекционных осложнений [6, 7]. Наиболее распространенным проявлением послеродовой инфекции считается эндометрит (Э). Частота заболевания после самопроизвольных родов составляет 3–5%, после кесарева сечения – 10–20%. Из 100 случаев послеродовых Э 80 возникают после кесарева сечения [8–10].
Цель данного исследования – клинико-эпидемиологическая характеристика факторов риска послеоперационного Э у родильниц на современном этапе развития службы родовспоможения.
Материалы и методы
Исследование выполнено на базе Урало-Сибирского научно-методического центра по профилактике инфекций, связанных с оказанием медицинской помощи (ИСМП) ФБУН «Екатеринбургский НИИ вирусных инфекций» Роспотребнадзора и кафедры эпидемиологии, социальной гигиены и организации госсанэпидслужбы ФГБОУ ВО «Уральский государственный медицинский университет» Минздрава России. В работе использованы данные как официальной регистрации ИСМП родильниц, так и дополнительные отчетные формы, разработанные авторами для учета и регистрации случаев ИСМП в медицинских организациях Свердловской области. Период наблюдения составил 28 лет (с 1991 по 2018 гг.). Всего проанализировано 16 413 случаев послеродовых инфекций родильниц, в том числе 3194 случая послеоперационных Э.
Для проведения мониторинга послеродовых Э начиная с 2010 г. в формы учета и регистрации были внесены изменения. Все Э были разделены на Э, развившиеся после родов через естественные родовые пути, и Э после кесарева сечения. Показатели заболеваемости рассчитывали следующим образом: заболеваемость послеродовым Э – на 1000 родов через естественные родовые пути, заболеваемость послеоперационным Э – на 1000 операций кесарева сечения.
Изучение факторов риска развития послеоперационного Э проведено на базе перинатального центра ГБУЗ СО «Областная детская клиническая больница № 1» (Екатеринбург), где были проанализированы 168 историй оперативных родов (форма 096/у), в том числе 82 – с физиологическим течением послеродового периода и 86 – с развитием Э.
Критерии включения в исследование: роды проходили в перинатальном центре, роды проводились путем кесарева сечения, диагноз Э поставлен в течение 30 дней с момента родоразрешения.
Критерии исключения из исследования: роды проходили в другом учреждении здравоохранения (не в областном перинатальном центре), роды проводились через естественные родовые пути, диагноз Э не поставлен (либо был снят).
Полученные данные были обобщены в несколько блоков, которые включали общие сведения о родильнице (фамилия; возраст; число родов, абортов и беременностей; срок гестации), сведения о родоразрешении (продолжительность безводного периода, инструментальные исследования, объем кровопотери), данные о наличии соматической и инфекционной патологии до и во время беременности и родов. У пациенток с Э были проанализированы данные о характере клинических проявлений заболевания.
В работе были использованы эпидемиологический и статистический методы исследования. Для анализа полученных данных определяли среднюю арифметическую величину (М) и стандартную ошибку показателя (m). Для оценки связи заболеваемости с предполагаемым фактором рассчитывали отношение шансов (OR), относительный риск (RR). Достоверность различий оценивали по критерию Фишера (φ) и t-критерию Стьюдента. Различия считали достоверными при р < 0,05.
Результаты
Областной перинатальный центр, функционирующий на базе ГБУЗ СО «Областная детская клиническая больница № 1» (далее – Центр), оказывает все виды высокотехнологичной медицинской помощи в области акушерства, гинекологии, неонатологии. Ежегодно в Центре проводится до 5000 родов, доля оперативных родов в среднем составляет 40,9%.
Средний многолетний уровень заболеваемости Э составил 24,2 ± 4,7‰, в том числе после родов через естественные родовые пути – 20,9 ± 4,1‰, после кесарева сечения – 30,2 ± 4,7‰. Изучение многолетней динамики показало, что уровень заболеваемости послеродовыми Э в Центре не имел значительных колебаний (18,1–27,8‰), тогда как заболеваемость послеоперационными Э имела выраженную тенденцию к росту с 22,4 до 50,7‰.
 В ходе исследования были подобраны 2 группы пациенток: в 1-ю вошли 86 родильниц с Э, во 2-ю – 82 родильницы без Э. Группы были репрезентативны по возрасту; числу беременностей, родов и абортов; срокам и количеству дней пребывания в Центре от поступления до выписки, от поступления до родов и от родов до выписки. Основную долю составляли женщины, у которых роды произошли на 39–40-й нед. гестации, доля родов на 35–38-й нед. составляла 26,7 ± 4,2%, на 22–34-й нед. – 12,8 ± 3,1%. Средняя продолжительность пребывания в роддоме составила от 6 до 7 дней, в том числе до родов – от 2 до 3 дней, после родов – от 3 до 4 дней (табл. 1).
В ходе исследования были подобраны 2 группы пациенток: в 1-ю вошли 86 родильниц с Э, во 2-ю – 82 родильницы без Э. Группы были репрезентативны по возрасту; числу беременностей, родов и абортов; срокам и количеству дней пребывания в Центре от поступления до выписки, от поступления до родов и от родов до выписки. Основную долю составляли женщины, у которых роды произошли на 39–40-й нед. гестации, доля родов на 35–38-й нед. составляла 26,7 ± 4,2%, на 22–34-й нед. – 12,8 ± 3,1%. Средняя продолжительность пребывания в роддоме составила от 6 до 7 дней, в том числе до родов – от 2 до 3 дней, после родов – от 3 до 4 дней (табл. 1).
Клинические проявления послеоперационного Э были типичными: патологические выделения из матки (15,1%), повышение температуры тела (14%), болезненность матки (10,5%), озноб (3,5%). Признаки заболевания в большинстве случаев (54,7%) имели место еще в период пребывания родильницы в Центре. Остальные случаи были выявлены на участке после выписки на 9–30-е сутки после родов.
У 60% заболевших женщин диагноз послеоперационного Э был подтвержден бактериологически выделением монокультур в 77% случаев, микробных ассоциаций – в 23%. В структуре монокультур преобладали грамотрицательные бактерии (57%), такие как Escherichia coli, Klebsiella pneumoniаe, Morganella morganii. У трети заболевших была выделена грамположительная микрофлора: Streptococcus agalactiae, Staphylococcus aureus, Staphylococcus epidermidis. В микробных ассоциациях также было отмечено преобладание грамотрицательной микрофлоры, что соответствовало специфике клинического процесса.
Среди заболеваний, перенесенных во время беременности, в группе родильниц с Э наиболее часто встречались заболевания органов малого таза (36,0%), что увеличивало вероятность развития Э в 7,1 раза.
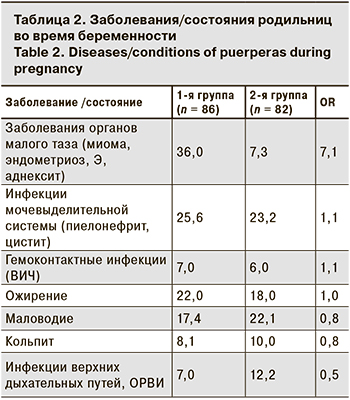 Инфекции мочевыделительной системы, ожирение, маловодие, инфекции верхних дыхательных путей и гемоконтаткные инфекции в обеих группах встречались с одинаковой частотой и не оказывали существенного влияния на развитие Э в послеродовом периоде (табл. 2).
Инфекции мочевыделительной системы, ожирение, маловодие, инфекции верхних дыхательных путей и гемоконтаткные инфекции в обеих группах встречались с одинаковой частотой и не оказывали существенного влияния на развитие Э в послеродовом периоде (табл. 2).
Установлено, что длительный (более 6 ч) безводный период увеличивал шанс развития послеоперационного Э в 1,5 раза. Инвазивные манипуляции во время родов и раннем послеродовом периоде также имели значительное влияние. Так, влагалищные исследования, проведенные в дородовом периоде и в родах от 2 до 4 раз, увеличивали шанс возникновения заболевания в 3,4 раза.
Дополнительным фактором, влияющим на частоту послеоперационного Э, было проведение кесарева сечения на вскрытом плодном пузыре (OR = 2,4) (табл. 3).
 Обсуждение
Обсуждение
Послеродовые гнойно-септические заболевания являются одной из актуальных проблем современного акушерства в связи с высокой частотой распространнения и постоянной тенденцией к росту заболеваемости. В течение последних 10 лет они устойчиво занимают 4-е место в структуре причин материнской смертности в мире [1, 6].
Учреждения родовспоможения Свердловской области не являются исключением. В них традиционно высок уровень регистрации ИСМП, в том числе ИСМП у родильниц: среднемноголетний показатель составил 13,32 ± 0,10‰. Послеродовые Э являются ведущей нозологической формой ИСМП, их доля в структуре гнойно-септических инфекций – 86,0–90,0%.
Многие авторы отмечают рост числа заболеваний родильниц, родоразрешившихся оперативным путем. Наиболее распространен Э, однако в ряде исследований отмечаются такие формы генерализованной послеродовой инфекции, как перитонит, сепсис, септический шок [4–8].
В нашем исследовании отмечен рост доли послеоперационных Э в структуре послеродовых инфекций полости матки с 26,6% в 90-е годы ХХ века до 40,8% в настоящее время (φэмп = 7,908; р < 0,01). Среднемноголетний показатель заболеваемости Э после оперативных родов в 1,8 раза превышал таковой при родах через естественные родовые пути: 18,42 ± 0,37‰ против 10,10 ± 0,18‰ (t = 20,22; р < 0,01).
Отмечено, что оперативное родоразрешение в 1,8 раза повышает риск развития тяжелых септических форм Э (RR = 1,825; 95% ДИ 1,732–1,924) и в 14 раз –послеродового сепсиса (RR = 12,109; 95% ДИ 6,331–23,157). Этот факт и определил необходимость более пристального изучения факторов риска развития послеоперационного Э в современных условиях.
Установлено, что клинические проявления послеоперационного Э типичны, признаки заболевания чаще всего (в 54,7% случаев) развиваются в первую неделю после родов. В структуре возбудителей, выделенных из патологического очага, преобладали грамотрицательные микроорганизмы, что несколько отличается от результатов других исследований [4, 6, 7].
В развитии Э важную роль играют факторы риска, имеющие место как во время беременности (бактериальный вагиноз, ИППП), так в родовом периоде (травмы мягких тканей, хориоамнионит, преждевременное излитие околоплодных вод) [8].
Дополнительными факторами риска развития послеоперационного Э являются заболевания органов малого таза (OR = 7,1), а среди факторов, связанных с оперативным вмешательством, – повторные влагалищные обследования (OR = 3,4), проведение операции на вскрытом плодном пузыре (OR = 2,4) при длительном безводном периоде (OR = 2,4).
Рост удельного веса оперативных родоразрешений, оправданный с точки зрения перинатальных рисков, неизбежно ведет к росту числа гнойно-воспалительных заболеваний родильниц. Это требует разработки новых подходов в реализации системы эпидемиологического надзора за ИСМП у родильниц с учетом факторов риска.
Выводы
Послеродовые Э составляют до 90% в структуре заболеваемости родильниц.
Факторами риска развития послеоперационного Э являются заболевания органов малого таза в период беременности (OR = 7,1); продолжительный безводный период (OR = 2,4); частые влагалищные исследования (более 1 в период родов) (OR = 3,4) и проведение кесарева сечения на вскрытом плодном пузыре (OR = 2,4).
Необходимо вносить изменения в действующую систему эпидемиологического надзора за ИСМП у родильниц с учетом современных факторов риска наиболее значимых нозологических форм (Э).