По данным Роспотребнадзора, в Российской Федерации сохраняется стабильно высокий уровень инфекционных заболеваний, связанными с оказанием медицинской помощи (ИСМП): за последние 10 лет регистрируется около 24 000–26 000 случаев в год или около 0,8 на 1000 госпитализаций1.
К ИСМП принято относить нозокомиальную пневмонию (НП), катетер-ассоциированные инфекции, в том числе инфекции кровотока и мочевых путей, постинъекционные инфильтраты – абсцессы и инфекции в области хирургического вмешательства и др., среди которых НП является наиболее частым инфекционным осложнением, ухудшающим прогноз и требующим дополнительных материальных затрат [1]. Диагноз НП устанавливают в соответствии с российскими и международными рекомендациями [2, 3]. Все случаи НП необходимо регистрировать2,3.
НП ассоциируется с высоким риском неблагоприятного исхода, особенно при развития заболевания на фоне продленной (более 48 ч) искусственной вентиляции легких (ИВЛ). Согласно данным мета-анализа, проведенного W.G. Melsen и соавт. [3], смертность среди больных с ИВЛ-ассоциированной НП (НПивл) составляет 7–30 %, при этом более высокий риск отмечен у пациентов хирургического профиля и больных, находившихся при поступлении в среднетяжелом состоянии.
Другим фактором риска при развитии НПивл является длительное пребывание больного в отделениях реанимации и интенсивной терапии (ОРИТ) [3]. У таких больных увеличивается вероятность развития инфекций различной локализации, обусловленных полирезистентными штаммами грамотрицательных патогенов, таких как Pseudomonas aeruginosa, Stenotrophomonas maltophilia и Кlebsiella pneumoniae, а также грамположительных – метициллин-резистентным Staphylococcus aureus (MRSA) [4 5]. В частности, у больных с НПивл в ОРИТ увеличивается частота встречаемости штаммов с резистентностью к цефалоспоринам III–IV поколения, фторхинолонам и карбапенемам [6–7].
Проблема выбора антибактериальной терапии (АБТ) становится все более значимой в условиях появления полирезистентных микроорганизмов и отсутствия новых антибактериальных препаратов (АБП) [8].
При НП выбор тактики АБТ зависит от сроков ее развития: при ранней НП, развивающейся в течение первых 4 дней от момента госпитализации, назначают традиционно используемые АБП, так как для этого периода характерны возбудители с хорошей чувствительностью к препаратам первого выбора. В случае развития поздней НП (более 4 дней от момента госпитализации) увеличивается риск инфицирования полирезистентными бактериями, что требует эмпирической АБТ с учетом локального микробиологического мониторинга [9].
В условиях роста поли- и панрезистентности бактерий для повышения эффективности АБТ следует проводить стратификацию риска полирезистентных инфекций с учетом анамнеза и особенностей предшествующей АБТ [3, 10].
Применять АБП нужно с учетом их фармакокинетических и фармакодинамических параметров, таких как продленная инфузия антисинегнойных бета-лактамов, однократное введение суточной дозы аминогликозидов, мониторирование остаточных и пиковых концентраций аминогликозидов и ванкомицина с последующим расчетом режима дозирования. Большое внимание уделяется ингаляционному пути введения антимикробных препаратов, который рассматривается как перспективный вариант, поскольку, с одной стороны, позволяет увеличивать концентрацию препарата в нижних дыхательных путях, с другой – характеризуется более низким риском развития нежелательных побочных реакций.
Учитывая высокий уровень летальности, особенно при НПивл, тяжелое течение заболевания и рост резистентности нозокомиальных возбудителей к АБП группы резерва, актуальным является выявление маркеров ранних предикторов развития НП, ее тяжелого течения, использование которых в клинической практике поможет снизить заболеваемость и улучшить прогноз для пациентов.
В связи с этим целью нашего исследования явилась оценка частоты встречаемости НП, анализ факторов риска неблагоприятного исхода и частоты выявления резистентных возбудителей у пациентов с НП в условиях многопрофильного стационара.
Материалы и методы
Проведен ретроспективный анализ историй болезни 700 пациентов терапевтического и хирургического профиля многопрофильного стационара за 2015 г.
Клиническими, рентгенологическими и лабораторными методами диагноз НП был подтвержден у 120 (17,1%) пациентов, среди которых было 63 мужчины и 57 женщин в возрасте от 29 до 93 лет. Средний возраст пациентов составил 63,4 ± 13,4 года: у мужчин – 62,8 ± 12,9 года, у женщин – 64,1 ± 13,9 года.
Для оценки факторов неблагоприятного прогноза были выделены 2 группы: пациенты с НП и с НПивл. Группы были сопоставимы по возрасту, полу, и индексу массы тела (ИМТ).
НПивл чаще встречалась в возрастной группе от 60 до 69 лет 22 – у 62,9% больных.
В отделениях хирургического профиля был зарегистрирован 101 случай НП. Все случаи НПивл были зарегистрированы у больных в позднем послеоперационном периоде. В отделениях терапевтического профиля было отмечено 19 (15,8%) случаев, при этом 3 (2,5%) пациентам из-за тяжелой дыхательной недостаточности было необходимо проведение ИВЛ. У больных терапевтических отделений все случаи НП также относились к позднему послеоперационному периоду.
Пациентам хирургических отделений были выполнены различные по профилю оперативные вмешательства: торакоабдоминальные – 35 (29,2%) больным, кардиохирургические – 32 (26,7%), сосудистые – 10 (8,3%), хирургия инфекционных осложнений – 14 (11,7%), торакальные – 3 (2,5%), урологические – 2 (1,7%), травматологические – 1 (0,8%), реконструктивные пластические – 4 (3,3%).
Был проведен анализ факторов риска, учитывали сопутствующие заболевания, предшествующую госпитализацию, прием АБП в последние 90 дней. При оценке факторов риска неблагоприятного прогноза учитывали факторы, приводившие к летальным исходам.
Анализировали результаты микробиологических исследований.
Статистическую обработку проводили с использованием языка R 3.3.24. Для непрерывных величин с нормальным распределением приводится среднее ± стандартное отклонение (M ± σ). Для величин с распределением, отличным от нормального, использовали медиану и 25,5 квартили. Для проверки нормальности распределения использовали формальный тест Шапиро–Уилкса. Для категориальных переменных приводятся абсолютное число и доля. Достоверность различий между группами оценивали с помощью t-критерия Стьюдента для непрерывных переменных с нормальным распределением; теста Вилкоксона – для переменных с распределением, отличным от нормального; критерия χ2 с поправкой Йетса на непрерывность или точного теста Фишера в зависимости от математического ожидания минимальной частоты в таблице сопряженности – для категориальных переменных.
Результаты и обсуждение
НП чаще развивается в послеоперационном периоде у больных хирургических отделений (84,2%) по сравнению с терапевтическими больными (15,8%).
По каждому случаю в базу данных вносили информацию о пациенте: пол; возраст; ИМТ; сведения о предшествующей госпитализации; приеме АБП в анамнезе; длительности пребывания в стационаре; тяжести состояния; наличии дыхательной недосаточности, потребовавшей респираторной поддержки; длительности ИВЛ; результатах микробиологических посевов; развитии других инфекционных и неинфекционных осложнений; проводимой АБТ, в том числе ингаляционной.
Больше всего летальных исходов было в возрастной группе от 60 до 69 лет – 13 (37,1%).
Частота развития НПивл была выше у больных после кардиохирургических и торакоабдоминальных вмешательств – 32 (26,7%) и 38 (31,7%) случаев соответственно. Объем оперативного вмешательства, длительность наркоза приводят к увеличению риска продленной вентиляции легких, что увеличивает риск развития трахеобронхита и НПивл.
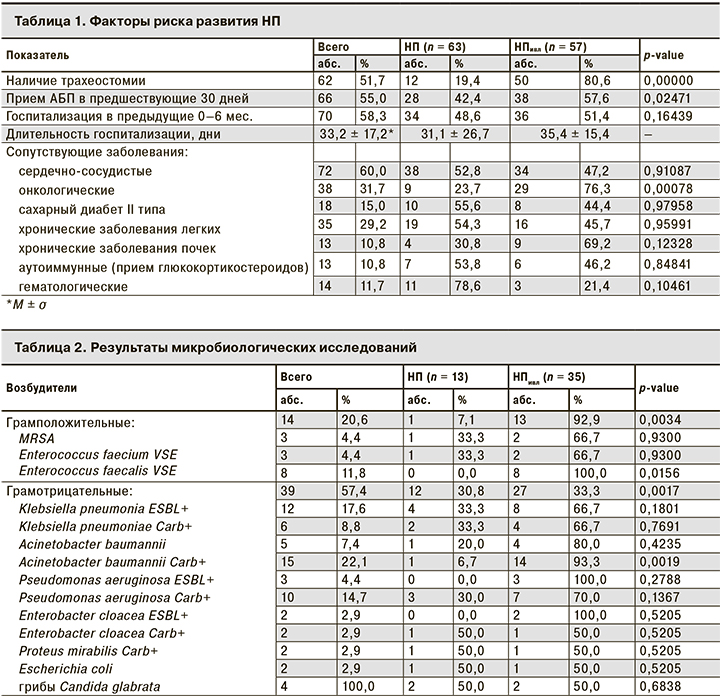
Был проведен анализ факторов риска развития НП, результаты которого представлены в табл. 1.
Мы не выявили достоверной связи между развитием НП и наличием сопутствующих патологий (p = 0,6707), таких как ХОБЛ (p = 0,9599), сахарный диабет II типа (p = 0,9796), сердечно-сосудистые (p = 0,91088), аутоиммунные (ревматоидный артрит, системная красная волчанка, первичный склерозирующий холангит; р = 0,8484) и гематологические (лимфогранулематоз, хронический миелолейкоз; р = 0,1046). Однако пациенты с онкологическими заболеваниями (рак пищевода, желудка, ободочной, прямой кишки, легких) находились в группе риска как развития НП, так и неблагоприятного исхода (р = 0,00078)
В соответствии Национальными рекомендациями [2, 10], по риску наличия резистентных возбудителей пациенты делятся на несколько типов:
I тип – отсутствие госпитализации за предыдущие 6 мес., приема АБП за последние 90 дней, сопутствующей патологии;
II тип – предыдущая госпитализация, прием АБП в течение 90 дней, сопутствующая патология;
III тип – длительная госпитализация, предшествующая АБТ, тяжелое течение основного заболевания;
IV тип – пациенты III типа с лихорадкой, отсутствием эффекта от адекватной АБТ, распространенная колонизация Candida spp, наличие факторов риска развития инвазивного кандидоза.
114 (95%) пациентов в нашем исследовании относились к III типу.
Были проведены микробиологические исследования мокроты, бронхоальвеолярной жидкости и крови у 62 (51,7%) пациентов, из них у 48 (40,0%) результаты оказались положительными (табл. 2).
Чаще всего выявляли полирезистентные патогены: Acinetobacter baumannii Carb+ – в 10 (14,7%) случаях, Pseudomonas aeruginosa Carb+ – в 10 (14,7%), Klebsiella pneumoniae ESBL+ – в 12 (25,0%), Klebsiella pneumoniae Carb+ – в 6 (12,5%). Среди грамположительных возбудителей преобладал Enterococcus faecalis VSE – 8 (11,8%) случаев (р = 0,0156). Можно сделать вывод, что среди возбудителей НП преобладают грамотрицательные микроорганизмы.
У пациентов с НПивл неблагоприятный прогноз был ассоциирован с увеличением длительности ИВЛ: в группе погибших она составила в среднем 13,5 дня (7–26,3 дня), в группе выживших – 1 день (0–6,4 дня; p = 4.9e-08). В группе больных с длительной ИВЛ была выше потребность в установке трахеостомы (60%; p = 6,9e-11).
Среди других предикторов неблагоприятного исхода отмечены предшествующая госпитализация (p = 0,006), потребность в проведении ИВЛ более 2 дней (p = 4,9e-08), онкологические заболевания (p = 0,00078).

Такие показатели, как ИМТ (27,0 ± 4,7 vs 26,8 ± 5,7; p = 0,88), длительность госпитализации (33,52 ± 18,79 дня vs 35,42 ± 22,33 дня; p = 0,7) не имели статистической значимости как факторы риска неблагоприятного исхода.
Следует отметить, что интубация и ИВЛ обычно способствуют снижению барьерных свойств организма, таким образом повышая риск развития НПивл. Баротравма, обусловленная ИВЛ, часто снижает уже нарушенную функцию легких. НПивл развивается примерно у трети пациентов, нуждающихся в ИВЛ в течение более 48 ч [11–13]. Кроме того, НП, развивающаяся у пациентов в условиях ОРИТ, связана с высокими показателями заболеваемости и смертности, поскольку эти пациенты соматически отягощены.
Мы проанализировали факторы неблагоприятного прогноза у больных, получавших комбинированную ингаляционную антибактериальную и парентеральную терапию. В результате пациенты, которым было необходима ингаляционная терапия, относились к группе крайне тяжелых пациентов, и, соответственно, выживаемость среди них была ниже (48%), чем в группе сравнения (72%; p = 0,03), что отражено в табл. 3.
В ходе лечения у пациентов в той или иной степени развивались как инфекционные, так и неинфекционные осложнения: острое почечное повреждение (ОПП) – у 46 (38,3%) больных: (увеличение креатинина сыворотки крови на 0,3 мг/дл (26,5 мкмоль/л) в течение 48 ч [14], послеоперационное кровотечение – у 16 (13,3%), тромбоэмболические осложнения – у 5 (4,2%), инфаркт миокарда – у 2 (1,7%). В послеоперационном периоде у 30 (25,0%) пациентов были отмечены нарушение ритма, гидро-, пневмоторакс, острый панкреатит, несостоятельность анастомозов, психомоторное возбуждение, которые также существенно осложняли течение заболевания.
Из 46 случаев ОПП 27 (58,7%) были отмечены в группе больных НПивл, а послеоперационные кровотечения среди больных НПивл и НП встречались в 12 (75,0%) и 4 (25.0%) случаях соответственно. У больных НПивл ожидаемо преобладала необходимость в вазопрессорной поддержке – 11(64,7%) случаев, а тромбоэмболические осложнения встречались в 4 (80,0%) случаях. ИСМП развивались чаще у пациентов с НПивл (23 случая; 82,1%) по сравнению с больными НП (5 случаев; 17,9%).
Наши данные согласуются с результатами многоцентрового клинического исследования, проведенного N. Sopena и соавт. [15], в котором летальность больных с НП достигла 36% и очень часто (52,1% случаев) НП протекала с тяжелыми осложнениями (острая дыхательная недостаточность, плевральный выпот, септический шок и др.).
Заключение
Проведенный ретроспективный анализ показал, что частота развития НП у больных, госпитализированных в отделения хирургического и терапевтического профиля многопрофильного стационара, составляет в среднем 17,1%.
Чаще всего НП имеет место у пациентов онкологического и кардиохирургического профиля.
Факторами риска неблагоприятного прогноза при НП являются онкохирургические заболевания, потребность в трахеостомии и длительность проведения ИВЛ более 2 дней.
Среди возбудителей инфекций наиболее резистентными оказались Pseudomonas aeruginosa, Klebsiella pneumoniae и Acinetobacter baumannii, что нужно учитывать при проведении АБТ, обусловленной тяжестью состояния пациента и необходимостью воздействия на полирезистентные микроорганизмы.
Таким образом, несомненна актуальность дальнейшей оптимизации фармакотерапии НП, создания алгоритмов АБТ и персонализированного подход к решению этой проблемы.