Болезни нервной системы являются одной из самых распространенных патологий, обуславливающих как временную, так и постоянную утрату работоспособности большого числа людей в мире. Согласно МКБ-10, класс болезней нервной системы (G00–G99) включает воспалительные, дегенеративные, демиелинизирующие заболевания, невропатии и параличи. Одновременно в неврологической практике особое внимание уделяется цереброваскулярной патологии, относящейся к болезням системы кровообращения (I00I99) и вносящей весомый вклад в уровни инвалидности и смертности населения [1].
На настоящий момент ведется поиск причин развития отдельных паталогических состояний в неврологии, в качестве которых рассматриваются различные инфекционные агенты, в том числе вирусы герпеса. В научной литературе приводятся сведения, что воспалительные заболевания нервной системы регистрируются на фоне активной инфекции, вызванной вирусами простого герпеса 1-го (ВПГ-1) и 2-го (ВПГ-2) типов [2], а также возбудителем ветряной оспы и опоясывающего лишая [3]. Описаны случаи менингоэнцефалита, развившегося у лиц с реактивацией ВПГ-2-инфекции [4]. Показано влияние ВПГ-1-инфекции на формирование очагов демиелинизации нервных волокон [5]. Установлена роль врожденной цитомегаловирусной инфекции (ЦМВИ) в развитии заболеваний центральной и периферической нервной системы от микроцефалии до потери слуха [6, 7]. Выявление ДНК вируса Эпштейна–Барр (ВЭБ) в спинномозговой жидкости пациентов с острым энцефалитом позволяет рассматривать данный патоген в качестве этиологического агента [8].
Одновременно вирусы герпеса рассматриваются в качестве триггерного фактора цереброваскулярной патологии. Так, при оценке влияния различных инфекционных агентов на развитие острого нарушения мозгового кровообращения у детей было установлено, что среди возбудителей вирусной природы превалировали вирусы герпеса [9]. Значительное число исследований посвящено роли ВПГ и возбудителя ветряной оспы в развитии цереброваскулярных болезней [10–12]. На основании оценки относительного риска (ОР) развития цереброваскулярной патологии у лиц с наличием и отсутствием маркеров ЦМВИ сделан вывод о роли данного возбудителя в развитии инсульта у женщин, при этом иные герпесвирусные инфекции (ГВИ) не изучались [13]. В литературе приводится описание клинических случаев инфаркта мозга и инсульта у взрослых и детей на фоне инфекции, вызванной вирусом герпеса человека 6-го типа (ВГЧ-6) [14, 15].
В то же время накопленные результаты исследований не дают однозначного ответа на вопрос о связи каждого из перечисленных возбудителей с конкретной патологией, поскольку являются преимущественно описаниями единичных клинических случаев, а методы доказательной статистики применяются весьма ограниченно.
Цель работы – определение роли ГВИ в формировании патологии нервной системы и сопряженных с ней цереброваскулярных болезней в ходе эпидемиологического исследования.
Материалы и методы
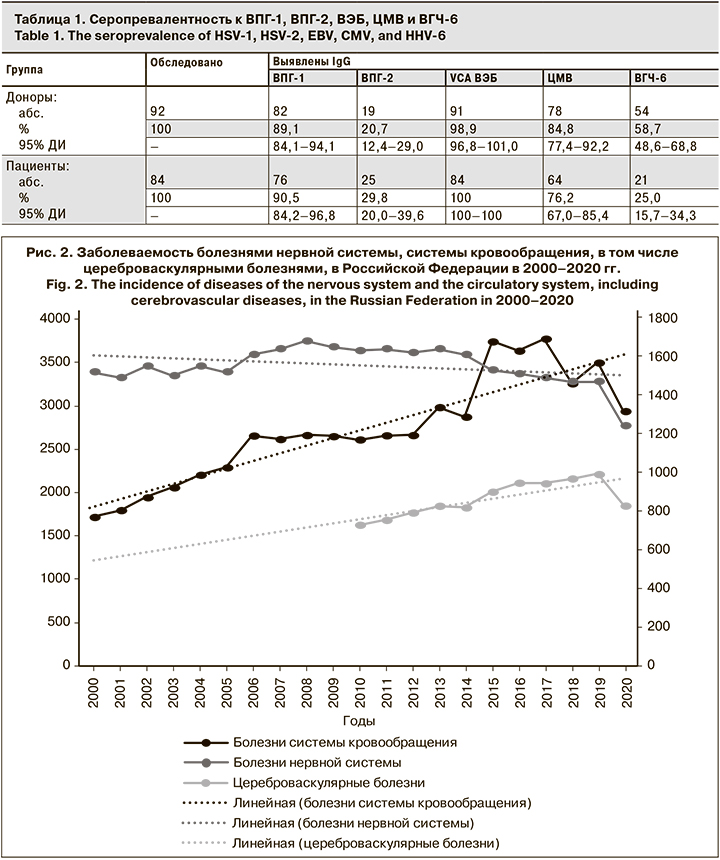
Исследование состояло из 2 этапов. На 1-м этапе ретроспективному анализу подвергнуты показатели заболеваемости населения Российской Федерации генитальным герпесом, инфекционным мононуклеозом, ЦМВИ, нервными болезнями и болезнями системы кровообращения, включая цереброваскулярные болезни, за период 2000–2020 гг. Источник данных – официальная отчетность Росстата [16–18].
Для определения характера связи использован коэффициент ранговой корреляции Спирмена (ρ). Связь считалась сильной при ρ ≥ 0,7, умеренной – 0,3 < ρ < 0,7, слабой – менее 0,3. Знаки «+» или «-» указывали на наличие прямой или обратной связи. Оценку достоверности связи проверяли путем нахождения табличного значения критической точки распределения Стьюдента (tкр) при р < 0,05 с последующим расчетом критического значения:
ρкр = tкр × √(1 - ρ2) / n - 2,
где n – объем выборки.
При условии ρ ≥ ρкр корреляционная связь считалась значимой.
На 2-м этапе исследовали сыворотки крови на наличие IgM и IgG к белкам ВПГ-1 и ВПГ-2, ВЭБ, ЦМВ, ВГЧ-6. Всего обследовано 176 чел. в возрасте от 18 до 65 лет, в том числе 92 донора крови и ее компонентов (далее – доноры) и 84 пациента неврологических отделений стационаров (далее – пациенты). Средний возраст пациентов составил 47,7 (95% ДИ 38,1–57,3), доноров – 41,0 (95% ДИ 35,8–46,2) года. В группе пациентов было 64,3% (95% ДИ 54,0–74,6) мужчин и 35,7% (95% ДИ 25,4–46,0) женщин; доноров – 66,3% (95% ДИ 56,4–76,2) и 33,7% (95% ДИ 23,8–43,6) соответственно. Из 84 пациентов 42 имели диагноз дорсопатии (код по МКБ-10 – М40–М54) и 42 – цереброваскулярной болезни (I60–I69).
Согласно решению локального совета по этике ФГБНУ НИИВС им. И.И. Мечникова, процедура исследования в соответствии с Хельсинкской декларацией не противоречит положениям биоэтики, поскольку от всех включенных в исследование лиц получено добровольное информированное согласие.
Идентификацию IgM и IgG к ВПГ-1, ВПГ-2 и ЦМВ; IgG к ВГЧ-6; IgM VCA, IgG VCA, IgG EA и IgG EBNA осуществляли методом ИФА с использованием наборов реагентов производства «Вектор–Бест» (Россия); обнаружение IgМ к ВГЧ-6 – непрямой реакцией иммунофлюоресценции (Euroimmun AG, Германия). Оценку результатов проводили согласно инструкциям по применению указанных наборов реагентов.
По каждому из исследуемых рядов данных оценивали нормальности распределения с использованием критерия Колмогорова–Смирнова по формуле:
К(λ) = Dmax × √N,
где Dmax – максимальная разница в накопленных эмпирических и теоретических частностях; N – число наблюдений в статистическом ряду. Во всех случаях распределение являлось нормальным, поскольку К(λ) < 1,36 при р < 0,05.
Для сопоставления полученных результатов рассчитывали частоту выявления серологических маркеров вирусов герпеса (%) и средние коэффициенты позитивности (КПср) для IgG ВПГ-1, ВПГ-2 и ВГЧ-6, IgG VCA и IgG EBNA ВЭБ. Достоверность различий оценивали с помощью 95% ДИ. Различия считали достоверными при р < 0,05.
При анализе риска развития неврологической патологии у пациентов (дорсопатии, цереброваскулярные болезни) использовался непараметрический критерий ОР. Значимость связи оценивали путем расчета стандартной ошибки и доверительного интервала (ДИ ОР). Связь признавалась статистически значимой, если ДИ ОР не включал в себя единицу.
Результаты
Ретроспективный анализ заболеваемости регистрируемыми ГВИ в Российской Федерации в 2000–2020 гг. выявил рост показателей инфекционного мононуклеоза и ЦМВИ и снижение генитального герпеса (рис. 1). В этот же период имели место рост заболеваемости болезнями системы кровообращения, в том числе цереброваскулярными болезнями, и снижение – болезнями нервной системы (рис. 2).
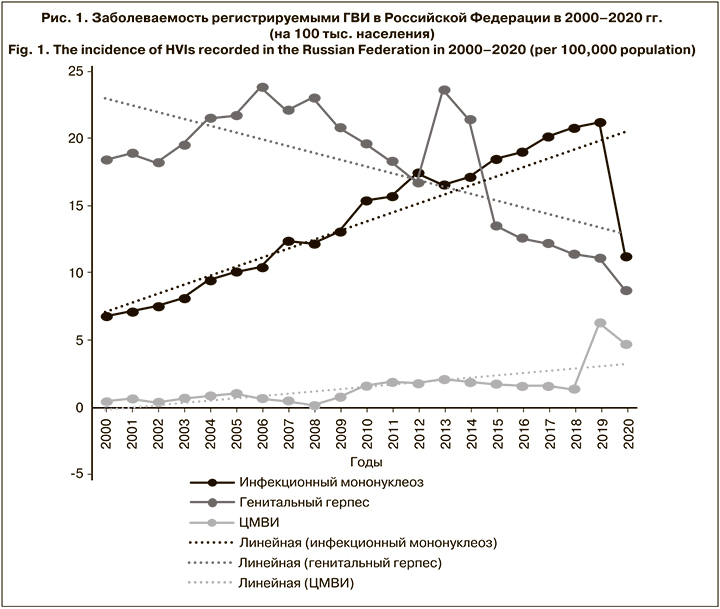
Сопоставление динамики заболеваемости регистрируемыми ГВИ, болезнями нервной системы, системы кровообращения, в том числе цереброваскулярными болезнями, за исследуемый период выявило наличие значимой сильной прямой корреляционной связи между следующими парами рядов:
- заболеваемость инфекционным мононуклеозом и болезнями системы кровообращения (ρ = 0,89; ρкр = 0,33);
- заболеваемость инфекционным мононуклеозом и цереброваскулярными болезнями (ρ = 0,92; ρкр = 0,51);
- заболеваемость генитальным герпесом и болезнями нервной системы (ρ = 0,70; ρкр = 0,40).
Анализ серопревалентности к исследуемым вирусам герпеса показал, что большинство участников исследования в обеих группах имели IgG VCA ВЭБ (табл. 1). Вторую позицию по частоте выявления как среди доноров, так и среди пациентов заняли IgG ВПГ-1, различия с показателями серопревалентности IgG VCA ВЭБ достоверны. Значимо реже у доноров выявляли IgG ВПГ-2, у пациентов – IgG ВПГ-2 и IgG ВГЧ-6. При сопоставлении показателей между группами установлено достоверное преобладание серопревалентности по IgG ВГЧ-6 в группе доноров (р < 0,05).
Для количественной оценки уровней IgG к вирусам герпеса использовали коэффициенты позитивности, оценка которых, согласно методике исследований, была проведена для IgG ВПГ-1 и ВПГ-2; IgG VCA и IgG EBNA ВЭБ; IgG ВГЧ-6 (табл. 2). В группе доноров КПср.. для всех указанных показателей были выше, чем в группе пациентов (различия достоверны для IgG ВПГ-1 и ВПГ-2, IgG EBNA ВЭБ, IgG ВГЧ-6; р < 0,05). Интерес представляют 2 показателя, характеризующие уровни IgG VCA и IgG EBNA ВЭБ. В группе доноров различия КПср данных маркеров отсутствуют, в то время как у пациентов КПср IgG EBNA достоверно ниже, чем IgG VCA (р < 0,05).
Анализ частоты выявления маркеров активной ГВИ показал значимое превышение IgM ВПГ-1 и ВПГ-2, Ig GEA ВЭБ, а также общей доли лиц с маркерами активной ВЭБ-инфекции в группе пациентов по сравнению с донорами (р < 0,05; табл. 3). В группе доноров показатели частоты выявления маркеров активной ГВИ были сопоставимы между собой. У пациентов достоверно чаще обнаруживали маркеры активной ВЭБ-инфекции – у 39,3% (95% ДИ 28,8–49,8). Для сравнения: следующие за ними IgM ВПГ-1 выявляли у 15,5% (95% ДИ 7,7–23,3), а IgM ВПГ-2 – у 10,7% (95% ДИ 4,1–17,3).

Анализ частоты выявления маркеров активной ГВИ в зависимости от патологии показал, что при активной ВПГ-1-инфекции достоверно чаще устанавливают диагноз дорсопатии, нежели цереброваскулярной болезни (р < 0,05). В равной степени обе патологии выявляют при наличии у пациентов IgM ВПГ-2 и IgM ВГЧ-6. У лиц с маркерами активной ВЭБ-инфекции (IgM VCA и IgG EA) чаще диагностируют цереброваскулярную патологию (р < 0,05).
Расчет ОР развития дорсопатий и цереброваскулярных болезней у лиц с маркерами активной ГВИ по сравнению с пациентами с неврологической патологией без ГВИ показал, что наличие IgM VCA и IgG EA ВЭБ статистически значимо (p < 0,05), повышает частоту развития цереброваскулярной патологии (ОР = 41,7; 95% ДИ 5,9–293,4). Несмотря на то что при активной ВПГ-1-инфекции диагноз дорсопатии устанавливают достоверно чаще, чем цереброваскулярной болезни, и показатель ОР превышает единицу, факт того, что наличие IgM ВПГ-1 увеличивает частоту развития дорсопатии, не является значимым, поскольку ДИ включает единицу (ОР = 1,2; 95% ДИ 0,9–1,5).
Обсуждение
Выдвинутое в настоящем исследовании исходное предположение о роли вирусов герпеса в развитии патологии нервной системы и сопряженных с ней цереброваскулярных болезней основывалось на данных, изложенных в отечественных и зарубежных публикациях. Учеными неоднократно предпринимались попытки установить этиологию отдельных нозологических форм, встречающихся в неврологической практике, используя результаты клинико-лабораторных и инструментальных исследований [2–15]. Однако именно клиническая направленность работ и незначительность выборок, по которым проводились наблюдения, не позволили до настоящего момента оценить роль этих патогенов в развитии исследуемой соматической патологии.
В настоящем эпидемиологическом исследовании впервые на основании большой статистической выборки определена роль отдельных ГВИ в формировании патологии нервной системы и сопряженных с ней цереброваскулярных болезней. В более ранних исследованиях выявлено наличие сильной прямой корреляционной связи между заболеваемостью инфекционным мононуклеозом и болезнями системы кровообращения [1]. В данной работе аналогичная корреляционная связь установлена для заболеваемости инфекционным мононуклеозом и цереброваскулярными болезнями, а заболеваемость болезнями нервной системы находилась в значимой сильной прямой зависимости от заболеваемости ВПГ-2-инфекцией. Отсутствие официального статистического учета случаев ВПГ-1- и ВГЧ-6-инфекции не позволило провести корреляционный анализ связи заболеваемости, вызванной этими вирусами герпеса, с исследуемой соматической патологией.
Еще более убедительные результаты получены при исследовании сывороток крови на наличие IgM и IgG к вирусам герпеса. Несмотря на то что уровни серопревалентности в группах условно здоровых лиц и пациентов неврологических стационаров в целом значимо не отличались и были сопоставимы с результатами других исследований [19], концентрации IgG ВПГ-1 и ВПГ-2, IgG EBNA ВЭБ и IgG ВГЧ-6 были достоверно выше в группе доноров. Полученные данные свидетельствуют о наличии более высокой иммунной защиты в группе условно здоровых, нежели у лиц с патологией [20], что дополнительно подтверждается достоверным преобладанием маркеров активной инфекции, вызванной ВПГ-1, ВПГ-2 и ВЭБ, у пациентов по сравнению с донорами.
Интересным представляется приоритет ВЭБ перед другими вирусами герпеса, заключающийся в достоверно более высоких показателях частоты выявления серологических маркеров, указывающих как на активную, так и на латентную инфекцию, по сравнению с ВПГ-1, ВПГ-2, ЦМВ и ВГЧ-6. При этом для маркеров латентной инфекции данная тенденция выявлена в обеих группах, а активной – только среди пациентов. Помимо достоверного превышения частоты выявления маркеров активной ВЭБ-инфекции у пациентов по сравнению с группой доноров, весомым аргументом в пользу того, что именно этот патоген играет триггерную роль в развитии исследуемой патологии, является значимое преобладание концентрации IgG VCA над IgG EBNA у лиц с наличием патологии. По данным ранее проведенных исследований, на фоне реактивации хронической ВЭБ-инфекции увеличение концентрации IgG VCA происходит раньше, чем IgG EBNA [21–23]. Окончательно убедиться в том, что именно активная ВЭБ-инфекция является значимым фактором риска развития цереброваскулярной патологии, позволяет оценка ОР (ОР 41,7; 95% ДИ 5,9–293,4), проведенная в ходе настоящего исследования.
Заключение
Таким образом, впервые показано, что перенесенная активная ВЭБ-инфекция является триггерным фактором развития цереброваскулярных болезней.