Генерализованная форма менингококковой инфекции (ГФМИ) характеризуется высоким уровнем летальности и длительным лечением даже при эффективной антибактериальной терапии и доступности интенсивной терапии [1, 2]. Возбудителем МИ является Neisseria meningitidis (менингококк) – грамотрицательный диплококк, облигатный патоген человека, который обычно колонизирует верхние дыхательные пути [3]. Менингококковая полисахаридная капсула является основным фактором вирулентности и основой классификации и номенклатуры бактерий, определяющей серогруппу [3]. Существует 12 менингококковых серогрупп: A, B, C, E, H, I, K, L, X, W, Y и Z. Половина из них (A, B, C, W, X и Y) ответственна почти за все случаи ГФМИ в мире с большим разбросом серогрупп по географическим регионам. ГФМИ поражает людей всех возрастов, особенно младенцев и детей младшего возраста, а также пожилых людей, среди которых показатели летальности высоки, часто из-за сопутствующих заболеваний [4]. Во многих странах также наблюдается небольшой пик заболеваемости ГФМИ в позднем подростковом и раннем взрослом возрасте [5]. ГФМИ обычно проявляется как менингит, сепсис или их комбинация; менее распространены пневмония, септический артрит, перикардит, эпиглоттит [6].
Уровень летальности при ГФМИ достигает 80% в нелеченных случаях и колеблется в пределах 4–20% при соответствующей терапии [7]. Более трети выживших после перенесенной ГФМИ имеют значительные осложнения, причем у 9% серьезные инвалидизирующие последствия остаются на всю жизнь [8, 9]. Летальность при ГФМИ является важным эпидемиологическим показателем для оценки бремени болезни, особенно в странах с массовой вакцинацией против МИ [10–12].
Цель исследования – характеристика структуры заболевших ГФМИ в РФ за период 2016–2019 гг. и определение частоты наступления летального исхода в зависимости от ряда факторов
Материалы и методы
Проанализированы данные о случаях ГФМИ из отчетной формы № 1, ежегодно пересылаемой в российский Референс-центр по мониторингу за бактериальными менингитами (РЦБМ) из управлений Роспотребнадзора по субъектам РФ и центров гигиены и эпидемиологии в субъектах РФ. Предоставление этих данных регламентировано информационными письмами Роспотребнадзора от 29.06.2010 № 01/9620-0-32 «О взаимодействии территориальных органов и учреждений Роспотребнадзора с Референс-центром по мониторингу за бактериальными менингитами» и от 13.06.2018 № 01/7608-2018-32 «О результатах мониторинга за заболеваемостью менингококковой инфекцией и бактериальными менингитами в Российской Федерации». Отчетная форма № 1 содержит персонифицированную информацию о заболевшем ГФМИ: пол, возраст, социальный статус, место жительства, данные о начале заболевания, дате госпитализации, первичном и окончательном диагнозе, исходе заболевания, а также лабораторном подтверждении случая. В РЦБМ в 2016–2019 гг. были предоставлены данные о 3027 больных. После исключения лиц с неизвестным исходом заболевания в исследование был включен 2961 пациент с окончательными диагнозом ГФМИ. Материал от 667 из 2961 больных (23,0%) дополнительно исследован в лаборатории РЦБМ. Для лабораторного подтверждения диагноза в РЦБМ использовали набор реагентов «АмплиСенс® NSH-FL» (ФБУН «Центральный НИИ эпидемиологии» Роспотребнадзора, Россия), серогруппирование N. meningitidis проводили c помощью набора реагентов «АмплиСенс® NmABCW-FL» того же производителя. Накопление, корректировку, систематизацию исходной информации и визуализацию полученных результатов осуществляли в электронных таблицах Microsoft Office Excel 2019.
Статистический анализ проводили, используя программы IBM SPSS Statistics v.26 (разработчик – IBM Corporation). Номинальные данные описывали с указанием абсолютных значений и процентных долей. Сравнение номинальных данных проводили при помощи критерия χ2 Пирсона и post hoc анализа. Рассчитывали показатель отношения шансов (ОШ) и границы 95% доверительного интервала (95% ДИ). Cилу связи между двумя категориальными полями измеряли с помощью критерия V Крамера.
Результаты
Среди заболевших в возрасте до 5 лет было 1398 (47,2%) человек, 5–14 лет – 459 (15,5%), 15–24 года – 438 (14,8%), 25–44 года – 363 (12,3%), 45–64 года – 241 (8,1%), старше 65 лет – 57 (1,9%). Данные о возрасте 5 заболевших утрачены. Женщины составили 45,2% (1337 человек), мужчины – 54,8% (1623 человека). Информация о половой принадлежности 1 пациента в РЦБМ не поступила. К городским жителям относились 2200 (74,3%) больных, в сельской местности проживали 689 (23,3%). Оставшиеся 2,4% составили лица с неуточненным местом проживания (72 заболевших).
В соответствии с социальным статусом больные распределились следующим образом: неорганизованные дети (дети, не посещающие детские дошкольные учреждения) – 1217 (41,1%) человек, учащиеся – 458 (15,5%), неработающие взрослые – 393 (13,3%), организованные дети – 388 (13,1%), работающие взрослые – 272 (9,2%), пенсионеры – 112 (3,8%), служащие – 67 (2,3%). Социальный статус 54 (1,8%) пациентов неизвестен.
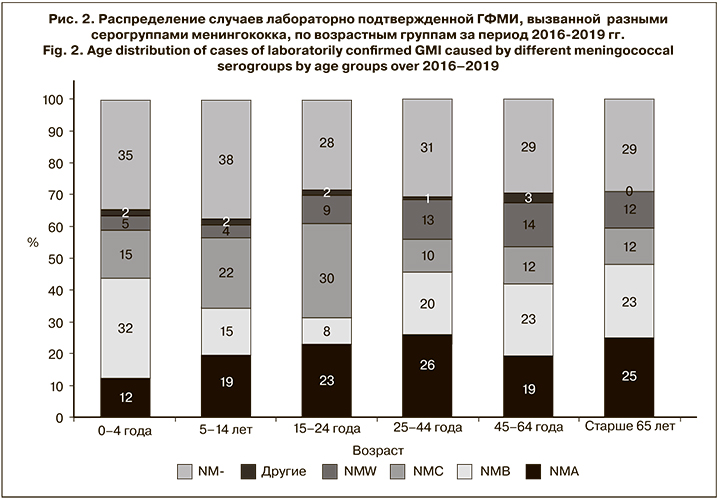
Диагноз ГФМИ был лабораторно подтвержден в 2183 случаях из 2961 (73,2%). В серогрупповой структуре доля Neisseria meningitidis серогруппы В (NMB) составила 22,5% (492 штамма), серогруппы А (NMA) – 18,0% (393), серогруппы С (NMC) – 17,5% (382), серогруппы W (NMW) – 7,5% (164), серогруппы Y (NMY) – 0,7% (15), NMW/Y – 0,9% (19), и 1 штамм принадлежал к серогруппе X. Информация о серогрупповой характеристике 717 (32,8%) штаммов в РЦБМ не поступила.
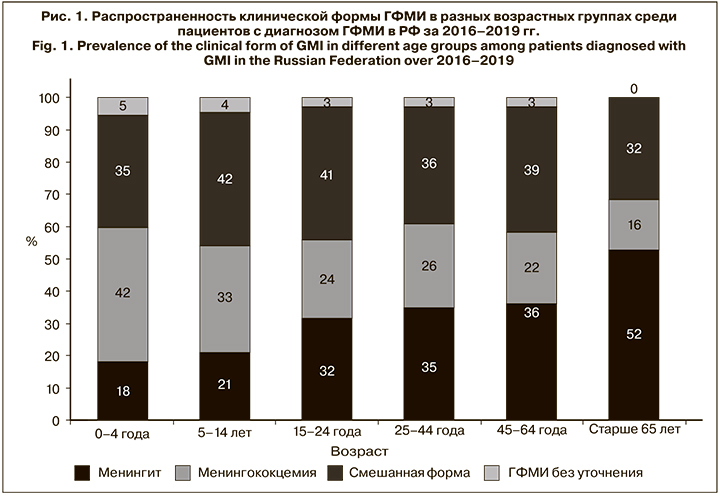
Среди клинических форм ГФМИ на смешанную форму (менингит и менингококцемия) приходилось 1103 (37,3%) случая, на менингококцемию – 998 (33,7%), на менингит – 731 (24,7%). В 129 (4,4%) случаях генерализованная форма заболевания осталась неуточненной. Достоверных различий серогруппового распределения среди клинических форм ГФМИ обнаружено не было.
Распределение клинических форм ГФМИ по возрастным группам представлено на рис. 1. Доля менингококцемии среди детей в группе 0–4 года составила 42% (581 случай) и с возрастом уменьшалась, достигая 16% (9 случаев) в группе пациентов старше 65 лет. Доля менингококкового менингита, напротив, с возрастом увеличивалась: среди детей в группе 0–4 года она составляла 18% (253 случая), возрастая до 52% (30 случаев) среди лиц старше 65 лет.
Распределение серогрупп менингококка среди госпитализированных пациентов с лабораторно подтвержденным диагнозом ГФМИ показало, что 296 (32%) случаев ГФМИ у детей в возрасте 0–4 года вызвал NMB, а в возрастной группе 15–24 года 111 (30%) случаев пришлось на долю NMC (рис. 2).
Из 2961 случаев ГФМИ 546 закончились летальным исходом. Общий показатель летальности составил 18% с максимальным значением в 2018 г. (20%). Он варьировал в зависимости от ряда факторов (см. таблицу).
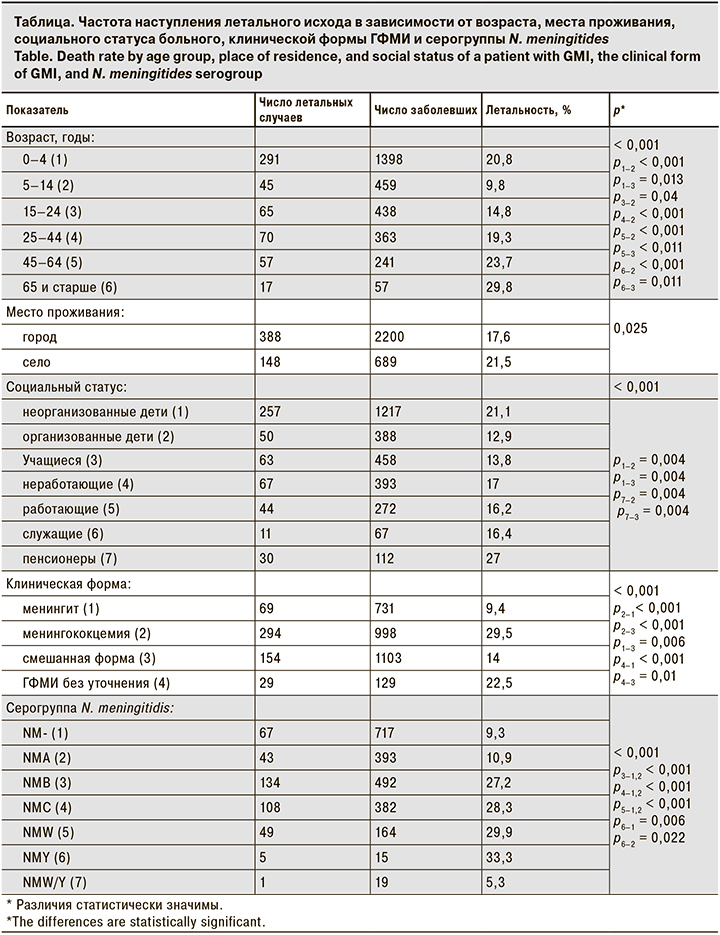
Более половины летальных случаев пришлось на долю детей в возрасте 0–4 года. Показатель летальности в этой группе составил 20,8%. При сравнении частоты летального исхода в разных возрастных группах были получены статистически значимые различия (р < 0,001), обусловленные более низкой частотой летального исхода в группах 5–14 лет (9,8%) по сравнению с остальными и 15–24 года (14,8%) по сравнению со всеми возрастными группами, кроме группы 25–44 года (19,3%).
Статистически значимых различий между полом заболевшего и летальным исходом не наблюдалось (р = 0,924). Частота летального исхода у женщин составила 18,5%, у мужчин – 18,4%.
При сравнении частоты летального исхода от ГФМИ и места жительства были получены статистически значимые различия (р = 0,025). Шанс летального исхода у городских жителей (17,6%) оказался в 1,3 раза ниже (ОШ – 0,781; 95% ДИ 0,632–0,966), чем у проживающих в сельской местности (21,5%).
Сравнение частоты летального исхода в зависимости от социального статуса выявило статистически значимые различия (р < 0,001). Летальный исход чаще отмечали среди лиц пенсионного возраста (27%), неорганизованных детей (21,1%) по сравнению с организованными (12,9%) и учащимися (13,8%), для которых были характерны самые низкие показатели летальности. Статистически значимых различий между показателями летальности в перечисленных группах и среди неработающих взрослых, работающих взрослых и служащих не выявлено.
Анализ частоты наступления летального исхода в зависимости от клинической формы ГФМИ показал статистически значимые различия (р < 0,001). Самый высокий уровень летальности установлен при менингококцемии (29,5%), самый низкий – при менингококковом менингите (9,4%). Между исходом заболевания и клинической формой ГФМИ отмечалась относительно сильная связь (V Крамера = 0,42).
При сравнении частоты летального исхода в зависимости от серогруппы N. meningitidis выявлены статистически значимые различия (р < 0,001). Более высокие показатели летальности отмечены для ГФМИ, вызванных серогруппами В (27,2%), С (28,3%), W (29,9%) и Y (33,3%) по сравнению с серогруппой А (10,9%) и негруппируемыми штаммамии (9,3%). Более высокие показатели p-value для серогруппы Y связаны с небольшим числом наблюдений в этой группе. Между сопоставляемыми признаками отмечалась средняя связь (V Крамера = 0,23). Достоверных различий между показателями летальности от ГФМИ, вызванных серогруппами В, С, W и Y, не наблюдалось.
Обсуждение
Коэффициент летальности в настоящем исследовании составил 18,4%, что выше аналогичных показателей в развитых странах.
В 2017 г. в Европейском центре по контролю и профилактике заболеваний (European Centre for Disease Prevention and Control – ECDC) был зарегистрирован 3221 подтвержденный случай ГФМИ в 30 странах Евросоюза, из них 282 (9,7%) случая закончились летальным исходом. Показатель летальности в странах Европы варьировал: во Франции – 11,6%, в Голландии – 8,3%, в Германии – 7,9%, в Португалии – 6,1%, в Испании – 9,1%, в Швеции – 20,4%, в Великобритании – 5,6% и т. д. [13].
В нашем исследовании частота летального исхода была связана с возрастом, социальным статусом, местом проживания больного, клинической картиной заболевания и капсульной группой менингококка.
Частота летального исхода с поправкой на возраст была статистически значимо ниже только у детей 5–14 лет. Дети, не посещающие детские дошкольные учреждения, погибали от ГФМИ статистически значимо чаще, чем организованные дети. Было установлено, что шанс летального исхода у сельских жителей в 1,3 раза выше, чем у городских. Это может быть связано с более поздним оказанием специализированной медицинской помощи. Показатель летальности с поправкой на клиническую форму болезни был самым высоким при менингококцемии, что согласуется с данными других исследований [14, 15] самым низким – при менингококковом менингите. Менингококки серогрупп В, С, W и Y одинаково ответственны за высокие показатели летальности, тогда как для ГФМИ, вызванной серогруппой А, показатель статистически значимо ниже.
Половина всех заболевших ГФМИ в РФ – дети в возрасте в возрасте 0–4 года. В этой группе наиболее высока доля ГФМИ, вызванных серогруппой В, а самая распространенная клиническая форма ГФМИ – менингококцемия. Каждый пятый случай заболевания закончился смертью ребенка. В то время как основной мерой борьбы против МИ во всем мире признана вакцинопрофилактика, в РФ она не включена в национальный календарь прививок. Вакцинация проводится лишь в соответствии с календарем прививок по эпидемическим показаниям, а также в очаге МИ. Это обстоятельство не позволяет говорить о возможности защиты всех детей. Данные исследования показывают, что более 1/3 случаев ГФМИ у детей можно было бы предупредить с помощью вакцинации, так как они были вызваны штаммами менингококка серогрупп A, C, W, Y, защита от которых предусмотрена составом зарегистрированной в РФ конъюгированнной вакцины. Причина еще 1/3 случаев заболевания у детей в возрасте 0–4 года – менингококк серогруппы В. Вакцина против ГФМИ, вызванной этим менингококком, не зарегистрирована в большинстве стран мира, в том числе в РФ. Глобальная экспертная группа наблюдения за МИ (Global Meningococcal Initiative – GMI) сообщает, что внедрение и использование субклеточных белковых вакцин против ГФМИ, вызванной менингококком серогруппы В, должно быть основано на молекулярном типировании циркулирующих в популяции штаммов. Необходимость такой рекомендации GMI связана с тем, что белковые вакцины могут не покрыть актуальные для определенной территории штаммы и тем самым не защитить от заболевания [16].
Заключение
Исследование показало, что каждый 5–6-й случай ГФМИ заканчивается летальным исходом. В этой связи целесообразно рассмотреть возможность включения в национальный календарь профилактических прививок плановой вакцинации детей против МИ, а в календаре прививок по эпидемическим показаниям расширить перечень категорий граждан, подлежащих обязательной вакцинации, в соответствии с санитарно-эпидемиологическими правилами СП 3.1.3542-18 «Профилактика менингококковой инфекции». Перспективным представляется изучение молекулярно-биологических свойств циркулирующих в стране штаммов менингококка серогруппы В. На основании полученных данных может быть рассмотрена степень охвата существующими менингококковыми вакцинами российских штаммов менингококка серогруппы В, и сделаны выводы о возможности их лицензирования в РФ.