Малярия – одно из наиболее широко распространенных и опасных инфекционных заболеваний [1–3]. По данным ВОЗ, ежегодно малярией болеют более 660 000 человек, около 330 000 из них погибают [4]. В Российской Федерации среди лиц, возвращающихся из эндемичных по малярии регионов, регулярно регистрируются случаи тропической малярии, вызываемой P. falciparum [1, 5–7]. При отсутствии своевременного адекватного лечения это заболевание может быстро прогрессировать и приводить к гибели пациентов [6, 8]. Одним из наиболее частых признаков злокачественного течения тропической малярии служит гемолитическая анемия, сопровождающаяся уменьшением количества эритроцитов и снижением уровня гемоглобина [8, 9]. Клетки крови разрушаются вследствие внедрения в них малярийных плазмодиев в процессе эритроцитарного цикла развития паразитов. Однако выраженность признаков анемии не всегда напрямую зависит от уровня паразитемии [9]. Даже при высокой концентрации паразитов в крови количество эритроцитов и уровень гемоглобина могут сохраняться в пределах физиологической нормы. Вместе с тем в отдельных случаях признаки тяжелой анемии регистрируются на фоне умеренной степени паразитемии, а уровень гемоглобина может снижаться даже после элиминации плазмодиев из крови [10]. Помимо непосредственного инфицирования эритроцитов малярийными плазмодиями наиболее вероятными причинами гемолитической анемии принято считать токсическое действие противомалярийных препаратов, а также аутоиммунные процессы [9]. Однако конкретные механизмы этого патологического процесса до конца не изучены.
В литературе высказываются предположения о том, что способность вызывать массовое разрушение неинфицированных эритроцитов является генетически детерминированным свойством отдельных штаммов P. falciparum [11–13]. Так, в последнее время появились сведения о наличии у P. falciparum генов, кодирующих специальные DBL-домены (Duffy-binding-like domains) [7, 14]. Эти структуры отличаются высокой полиморфностью и входят в состав наиболее вариабельной части главного фактора вирулентности P. falciparum (PFEMP1). Установлено, что домены типа DBL1α и DBLß обладают высокой тропностью к рецептору комплемента 1 (complement receptor 1 – CR1), известному как рецептор C3b/C4b или CD35 (кластер дифференциации 35) [7, 13]. В результате взаимодействия CR1 со структурами PFEMP1 активируется система комплемента, что может инициировать развитие аутоиммунного процесса и, как следствие, вызвать массовую гибель неинфицированных клеток крови. В настоящее время структура генома P. falciparum полностью расшифрована. В частности выявлены нуклеотидные последовательности генов групп upsB и upsC, которые кодируют полипептиды доменов DBL1α и DBLß, а также других функциональных участков PFEMP1 (DBLγ, DBLδ, DBLε, DBLζ, CIDRα, CIDRβ, CIDRγ и др.) [15–17]. Подобраны праймеры для идентификации соответствующих маркерных участков генома паразитов [13].
Предположения о возможной генетической детерминированности клинических проявлений малярийной инфекции основываются на результатах обширных экспериментальных исследований, проведенных с использованием биологических моделей [7, 11]. Клинических наблюдений, подтверждающих связь между развитием тяжелой анемии и особенностями строения генома P. falciparum, пока недостаточно. В Российской Федерации подобные исследования еще не проводились. В связи с этим приобретает актуальность изучение молекулярно-генетических особенностей штаммов P. falciparum, вызывающих случаи тропической малярии с разными формами клинического течения заболевания.
Цель работы – изучение генотипических особенностей Plasmodium falciparum при тяжелой форме тропической малярии, осложненной гемолитической анемией.
Материалы и методы
Материалом для исследования послужили 2 случая тропической малярии, выявленных в стационарах Санкт-Петербурга в 2018 г. В одном случае заболевание протекало тяжело и сопровождалось развитием тяжелой анемии, в другом случае оно протекало без осложнений.
Клиническое наблюдение 1.
Больной В., 29 лет, житель Санкт-Петербурга. 5.10.2018 возвратился из поездки в Буркина-Фасо (Западная Африка). В период пребывания в Африке профилактического противомалярийного лечения не получал. Считает себя больным с 11.10.2018, когда отметил повышение температуры тела до 39,9 °С. Получал амбулаторное лечение по поводу острого респираторного заболевания. На фоне приема жаропонижающих препаратов отмечал ухудшение состояния, наблюдались озноб, лихорадка до 39,0–40,2 °С, профузное потоотделение в ночное время, нарастала слабость. На 6-й день экстренно госпитализирован в инфекционный стационар, где в приемном покое при паразитологическом исследовании в крови обнаружены возбудители тропической малярии (P. falciparum, юные трофозоиты, более 5000 в 1 мкл).
При поступлении состояние тяжелое. Больной вял, адинамичен. Кожа бледная с желтушностью, сосуды склер инъецированы. Дыхание учащенное, 18–20 в минуту. Тоны сердца приглушены, пульс учащен, 110–120 в минуту. Артериальное давление – 70 на 40 мм рт. ст. Печень пальпируется на 4 см ниже края реберной дуги, селезенка увеличена. При лабораторных исследованиях выявлены признаки гемолитической анемии: количество эритроцитов соответствует нижней границе нормы (4,07 × 1012/л), уровень гемоглобина снижен (116 г/л), тромбоцитопения (50 × 109/л), повышен уровень трансаминаз (АЛТ – 174,8 Ед/л, АСТ – 175,9 Ед/л). Также повышены показатели билирубина (86,2 мкмоль/л) и креатинина (123,4 мкмоль/л). Содержание глюкозы низкое (до 2,97 ммоль/л). Моча коричневая, ее плотность снижена (1,00), при микроскопии выявляются эритроциты (25 в 1 мкл) и лейкоциты (25 в 1 мкл). Регистрируются протеинурия (0,25 г/л) и билирубинурия (17 ммоль/л).
Больной был направлен в отделение реанимации и интенсивной терапии (ОРИТ), назначено противомалярийное лечение (комбинированный препарат артеметер 20 мг и люмефантрин 120 мг), начата патогенетическая терапия. На фоне проводимого лечения состояние пациента улучшилось. Температура тела нормализовалась на 3-й день этиотропной терапии. Положительная динамика заболевания послужила поводом для перевода больного в инфекционное отделение. Уровень паразитемии прогрессивно снижался, и к 8-м суткам терапии паразиты в препаратах крови не выявлялись. Уровень гемоглобина продолжал снижаться и на 9-й день составил 84 г/л. Нарастала общая слабость, сохранялась желтуха. При лабораторном обследовании моча красного цвета, в осадке выявлены эритроциты (75 в 1 мкл) и лейкоциты (50 в 1 мкл). Регистрируется протеинурия (5 г/л). Снижение уровня гемоглобина (до 50 г/л) и количества эритроцитов (до 1,75 × 1012/л) потребовало повторного перевода пациента в ОРИТ, где начато введение кровезамещающих препаратов и гемотрансфузии. В результате к 12-му дню состояние больного стабилизировалось. В дальнейшем заболевание протекало без особенностей, клиническая картина характеризовалось постепенным улучшением самочувствия, восстановлением клинико-лабораторных показателей. Пациент был выписан с выздоровлением на 29-й день стационарного лечения после трехкратных отрицательных результатов паразитологического исследования крови.
Развитие тропической малярии у больного В. характеризовалось тяжелым течением, осложненным гемолитической анемией, острым канальцевым некрозом токсического генеза (Hb), острым повреждением почек I стадии.
Клинический случай 2.
Больной М., 24 года, студент одного из вузов Санкт-Петербурга. Летом посетил Республику Руанда, 3.09.2018 возвратился в Санкт-Петербург. Через 10 дней почувствовал головную боль, общую слабость, лихорадку (39,0 °С). Госпитализирован в инфекционный стационар с диагнозом «острое респираторное заболевание». При поступлении общее состояние удовлетворительное, носовое дыхание затруднено, с незначительными слизистыми выделениями. На фоне приема жаропонижающих препаратов сохранялся субфебрилитет. Пульс – 70–72 в минуту, ритмичный; артериальное давление – 105–110 на 70–75 мм рт. ст. На 3-й день заболевания зарегистрировано ухудшение самочувствия, повышение температуры тела до 38,5 °С, сопровождавшееся головной болью, слабостью, болями в мышцах. Учитывая эпидемиологический анамнез, проведено паразитологическое исследование, в ходе которого в крови пациента выявлены возбудители тропической малярии (P. falciparum, юные трофозоиты, более 5000 в 1 мкл). Больной был переведен в ОРИТ, назначено противомалярийное лечение (комбинированный препарат артеметер 20 мг и люмефантрин 120 мг), начата комплексная патогенетическая терапия. Субъективные признаки заболевания исчезли в течение 2 дней. На 5-е сутки после начала этиотропной терапии больной переведен в инфекционный стационар. На фоне проводимого лечения количество паразитов в крови прогрессивно снижалось, а начиная с 6-го дня плазмодии в препаратах крови микроскопически не выявлялись. Температура тела нормализовалась через сутки после начала лечения. Изменения со стороны органов и систем не выявены, печень и селезенка не увеличивались. Признаков анемии не установлено. Количество эритроцитов существенно не менялось и составляло 4,9–5,3 × 1012/л, уровень гемоглобина изменялся незначительно и составлял 137–149 г/л. Пациент выписан с выздоровлением на 10-й день после трехкратного отрицательного результата микроскопического исследования крови.
Заболевание у больного М. характеризовалось среднетяжелым течением без осложнений.
Для проведения молекулярно-генетических исследований использовали технологию полимеразной цепной реакции (ПЦР). Материалом служила высушенная кровь со стекол, приготовленных для препарата «толстая капля». В работе использовали пробы крови, взятой у пациентов в момент поступления в стационар. ДНК из проб крови выделяли, соскабливая материал со стекол с последующей его гомогенизацией в 300 мкл TES буфера в эппендорфах. Смесь нагревали на водяной бане при 99 °С в течение 5 мин. Материал ресуспендировали, остужали до комнатной температуры и центрифугировали при 12 000 об/мин в течение 2 мин. Надосадочную жидкость отбирали для дальнейших исследований.
 При проведении ПЦР использовали амплификатор Biorad С1000. Реакционная смесь включала следующие реактивы: деионизированная вода – 5,2 мкл, 5x Taq Red буфер (ЗАО «Евроген», Россия) – 2 мкл, dNTPs (ЗАО «Евроген», Россия) – 1,2 мкл 2,5 мМ, прямой и обратный праймеры – по 0,2 мкл 20 мкМ, Taq-ДНК-полимераза (НПО «СибЭнзим», Россия) – 0,2 мкл, 1 U, матрица выделенной ДНК – 1 мкл.
При проведении ПЦР использовали амплификатор Biorad С1000. Реакционная смесь включала следующие реактивы: деионизированная вода – 5,2 мкл, 5x Taq Red буфер (ЗАО «Евроген», Россия) – 2 мкл, dNTPs (ЗАО «Евроген», Россия) – 1,2 мкл 2,5 мМ, прямой и обратный праймеры – по 0,2 мкл 20 мкМ, Taq-ДНК-полимераза (НПО «СибЭнзим», Россия) – 0,2 мкл, 1 U, матрица выделенной ДНК – 1 мкл.
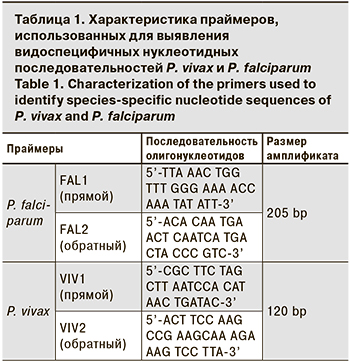
Для молекулярно-генетического подтверждения видовой принадлежности возбудителей использовали видоспецифичные праймеры P. vivax и P. falciparum к гену 18S РНК паразитов (табл. 1).
Режимы этапов амплификации:
- Начальная денатурация – 95 °С, 5 мин.
- Основная денатурация – 94 °С, 15 с.
- Отжиг праймеров – 58 °С, 30 c.
- Элонгация – 72 °С, 15 c.
- Финальная элонгация – 72 °С, 8 мин.
Этапы со 2-го по 4-й повторяли циклически 35 раз.
Для выявления участков генома P. falciparum, синтезирующих белки, специфичные к рецептору комплемента, использовали праймеры к маркерным нуклеотидным последовательностям, кодирующим структуру доменов DBL1α и DBLβ [14]. Дополнительно использовали праймеры к генам, кодирующим домен CIDR1α [14], в отношении которого отсутствуют сведения о его способности взаимодействовать с CR1 и другими факторами активации системы комплемента [8, 11, 18]. Характеристика праймеров, использованных для амплификации маркерных участков генома паразитов, представлена в табл. 2.

Режимы этапов амплификации:
- Начальная денатурация – 95 °С, 5 мин.
- Основная денатурация – 95 °С, 30 с.
- Отжиг праймеров – температура отжига (Ta, °С – см. табл. 2), 1 мин.
- Элонгация – 64 °С, 30 c.
- Финальная элонгация – 72 °С, 5 мин.
Этапы со 2-го по 4-й повторяли циклически 35 раз.
Продукты амплификации разделяли посредством электрофореза на 2% агарозном геле с использованием электрофоретической камеры Sub-Cell GT (Bio-Rad, США). Использовали агарозу LE (Termofisher), разведенную на TBS-буфере с добавлением этидия бромида (biotechnology Grade). Размер амплифицированных участков ДНК оценивали с помощью стандартных маркеров длины ДНК (100 bp и 50+ bp DNA Ladder). Результаты электрофореза учитывали с помощью трансиллюминатора Vilber Lourmat ECX-20M (Vilber Lourmat, Франция). Результаты фиксировали с помощью системы гель-документации.
Результаты
При микроскопическом исследовании препаратов «толстая капля» и «тонкий мазок» в крови пациентов В. и М. были выявлены юные трофозоиты P. falciparum. Концентрация паразитов в обеих пробах составила более 5000 паразитов в 1 мкл крови (рис. 1, 2, см. на вклейке). Это подтвердило результаты исследований, проведенных в стационаре.
Результаты ПЦР с видоспецифичными праймерами подтвердили присутствие в пробах крови пациентов В. и М. нуклеотидных последовательностей, характерных для генома P. falciparum. При этом амплификация с праймерами к гену 18S РНК P. vivax в обоих случаях дала отрицательные результаты (табл. 3).
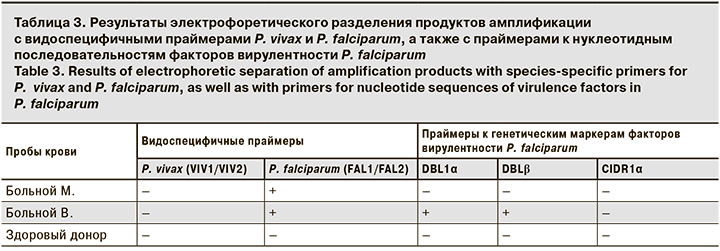
Исследование проб с использованием праймеров к различным регионам var-комплекса P. falciparum показало, что реакции с кровью пациента В. давали положительные результаты на нуклеотидные последовательности, соответствующие как домену DBL1α, так и домену DBLβ. В то же время соответствующие исследования образцов крови пациента М. показали отрицательный результат. По результатам ПЦР с применением праймеров к нуклеотидным последовательностям домена CIDR1α в пробах крови обоих пациентов маркерные участки var-комплекса, кодирующие область домена CIDR1α, не выявлены.
Таким образом, заболевание тропической малярией у пациента В., при котором выявляли генетические маркеры PFEMP1, соответствующие доменам DBL1α и DBLβ, сопровождалось развитием осложнений – гемолитической анемии и острого почечного повреждения. При этом клинические проявления характеризовались субъективными ощущениями тошноты, выраженной слабости, головной боли, а также объективными признаками желтушности кожи и склер, гепато- и спленомегалии. Среди лабораторных признаков анемии наибольшее значение имело уменьшение количества эритроцитов, снижение уровня гемоглобина, тромбоцитопения, повышение уровня трансаминаз, билирубина, креатинина, а также протеинурия, микрогематурия и билирубинемия.
Во втором клиническом случае заболевание протекало без осложнений. При этом ПЦР с пробами крови пациента М. давала отрицательные результаты на генетические маркеры паразитарных белков, специфичных к рецептору комплемента.
Обсуждение
Исследованные генетические маркеры вирулентности P. falciparum в перспективе могли бы рассматриваться в качестве ранних предикторов злокачественного течения тропической малярии, однако, единичное наблюдение не дает оснований для практических рекомендаций. Поэтому прикладное практическое значение полученных результатов в настоящей работе не обсуждается.
Вместе с тем полученные результаты могут рассматриваться как попытка объяснить механизм острой почечной недостаточности при злокачественном течении тропической малярии. В настоящее время объяснение причин этого осложнения, как правило, ограничивается системными патологическими процессами (изменение гемодинамики, гиперпаразитемия, диссеминированное внутрисосудистое свертывание крови, массивный гемолиз, гемоглобинурия) [9, 19], а также механизмами, развивающимися на тканевом и клеточном уровнях (адгезия и секвестрация пораженных эритроцитов, скопление лейкоцитов в клубочковых и перитублярных капиллярах) [20, 21]. Молекулярно-генетические механизмы нефротоксического действия P. falciparum до настоящего времени подробно не обсуждались.
Полученные результаты дают основание рассматривать развитие тяжелых форм малярии не просто как спорадическое явление, зависящее исключительно от восприимчивости макроорганизма и развивающееся вследствие несвоевременного или неадекватного этиотропного лечения [9, 19, 22]. Выявление генетических маркеров вирулентности паразитов позволяет предположить, что развитие тяжелых осложненных форм малярии во многом зависит от индивидуальных генетических особенностей возбудителей и, в частности, от наличия или отсутствия в их геноме нуклеотидных последовательностей, кодирующих специфические белки в составе главного фактора вирулентности P. falciparum. Штаммы паразитов, var-комплекс которых включает регионы upsB-type 5 UTR и upsC-type 5 UTR, а PFEMP1 содержит домены DBL1α и DBLβ, могут способствовать тяжелому течению заболевания и провоцировать развитие гемолитической анемии.
Выявленные в настоящем исследовании генетические различия возбудителей на фоне злокачественного и неосложненного течения тропической малярии подтверждают предположение о генетической гетерогенности популяции малярийных плазмодиев как основы саморегуляции паразитарных систем [22, 23].
Заключение
Анализ результатов проведенных исследований дает основание предполагать наличие связи особенностей генома P. falciparum с клиническим течением тропической малярии. Дальнейшее изучение динамики циркуляции фрагментов генома P. falciparum в крови больных тропической малярией может быть использовано в клинической практике для прогноза развития заболевания. Исследование генетического профиля P. falciparum (генетической гетерогенности var-гена) может служить методологической основой для изучения фазовых преобразований вирулентности паразитов, а также механизмов саморегуляции и устойчивости паразитарных систем малярии.