Лабораторная диагностика рецидивирующих респираторных инфекционно-воспалительных заболеваний (РИВЗ), наряду с традиционными инструментальными методами обследования и общим анализом крови, включает специфические анализы на выявление возбудителя – серологические и микробиологические тесты. Исследование микробиоты чаще всего сводится к бактериологическим посевам отделяемого из носа, бронхов и ротоглотки. Посев из ротоглотки является достаточно показательным тестом, поскольку микробиота данного локуса во многом определяется затёком отделяемого из носовой полости и попаданием секрета из нижних дыхательных путей при кашле. Состав эу- и прокариотных микроорганизмов ротоглотки, встречающихся при разных нозологических формах РИВЗ изучали разные исследователи [1–9]. Установлено, что он варьирует в зависимости от географического расположения страны и методов исследования, но, как правило, сводится к нескольким типам (Phyla) бактерий: Firmicutes, Fusobacteria, Bacteroidetes, Proteobacteria и Actinobacteria. Внедрение молекулярных методов значительно расширило спектр микроорганизмов, обнаруживаемых в ротоглотке, однако превалирующие виды остаются примерно теми же – это золотистый стафилококк и некоторые виды стрептококков. Но помимо видового/родового состава микроорганизмов и их количественной характеристики для назначения адекватной антибиотикотерапии клиницисту важно знать спектр антибиотикочувствительности выделенных от пациента условно-патогенных микроорганизмов, в чем молекулярные методы рутинного характер помочь не могут. На основании получаемых в микробиологической лаборатории данных необходимо периодически проводить мониторирование как видового состава, так и чувствительности/резистентности микроорганизмов к набору антибиотиков, так как это дает возможность назначения адекватной антибактериальной терапии в короткие сроки без предварительного бактериологического исследования. В связи с вышеизложенным целью настоящего исследования явилось изучение видового состава и антибиотикочувствительности микробиоты ротоглотки при РИВЗ.
 Материалы и методы
Материалы и методы
В исследование были включены 189 человек в возрасте от 1 года до 46 лет, прошедших обследование в консультативно-поликлиническом отделении при ФГБНУ «Научно-исследовательский институт вакцин и сывороток имени И.И.Мечникова» за период с 2013 по 2016 г. Критерием включения явилось наличие РИВЗ Диагнозы выставлялись клиницистами в соответствии с МКБ-10.
Мазки производили стерильными ватными тампонами с задней стенки глотки и поверхности миндалин. Тампоны помещали в транспортную среду и доставляли в лабораторию, где проводили посевы на чашки с селективными средами: Эндо, Сабуро, желточно-солевым агаром, кровяным агаром и шоколодным агаром. Чашки инкубировали в термостате в течение 1–2 суток в зависимости от среды, после чего появившиеся колонии подсчитывали и проводили идентификацию аэробных и факультативно-анаэробных микроорганизмов с помощью стандартных физиолого-биохимических тестов (ассимилляция углеводов и других субстратов, наличие ферментативной активности уреазы, каталазы, оксидазы и др., окрашивание по Граму и микроскопирование) [10–13].
Чувствительность возбудителей к антибиотикам определяли дискодиффузионным способом по усовершенствованному методу Керби–Бауэра с помощью стандартных дисков с антибиотиками [14]. Статистическую обработку данных проводили с использованием программы Microsoft Excel.
Результаты и обсуждение
Спектр рецидивирующих РИВЗ в группе обследованных представлен на рис. 1. (см. на вклейке). Видно, что лидирующие позиции занимали хронический ринит/хронический ринофарингит, аллергический ринит и острый назофарингит; гораздо реже встречались болезнь аденоидов/миндалин, бронхиальная астма, хроническая обструктивная болезнь легких и ангина/острый тонзиллит.
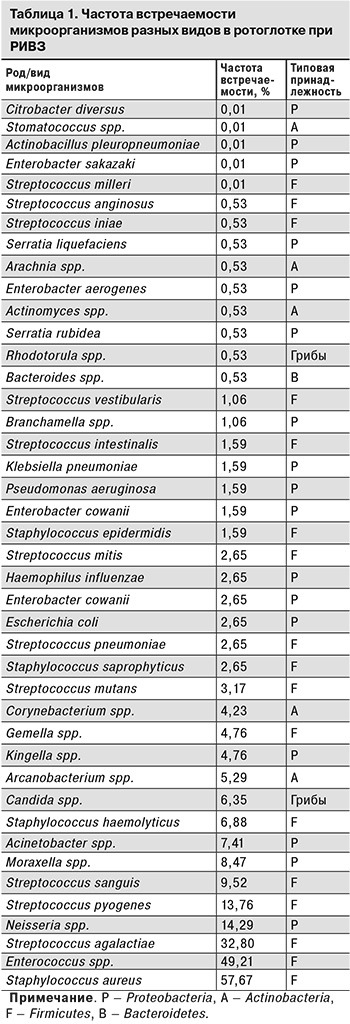
В результате обследования 189 пациентов получено 495 изолятов, которые классическими методами удалось идентифицировать до уровня рода (25 родов) или вида (28 видов). Результаты идентификации выделенных штаммов микроорганизмов представлены в табл. 1. Наиболее часто встречались (в порядке убывания): Staphylococcus aureus (S. aureus), Enterococcus spp., Streptococcus agalactiae (Str. agalactiae), Neisseria spp. и Streptococcus pyogenes (Str. pyogenes). Прочие роды встречались не чаще, чем в 10% случаев. Данные, полученные другими исследователями при изучении традиционными методами микрофлоры небных миндалин у больных хроническим тонзиллитом, показали сходные результаты: носителями золотистого стафиллококка являлись от 39,7% [3] до 75,9% пациентов [2]. В другом аналогичном исследовании [1] первое место занимали стрептококки (40,0%), второе – S. aureus (28,9%). Поскольку в изученных нами образцах вследствие затёка отделяемого из носовой полости могли обнаруживаться нетипичные для миндалин микроорганизмы, следовало сравнить полученные результаты с таковыми при рините (риносинусите). По данным исследователей, S. aureus и Pseudomonas aeruginosa [6] или S. aureus и Propionibacterium acnes [4, 7] являются причинно-значимыми микроорганизмами в развитии тяжелых форм риносинусита.
В табл. 1 представлено также распределение изолятов бактерий по типам (Phyla): простой подсчет показывает, что 74,4% из них принадлежало к типу Firmicutes, тогда как к Proteobacteria – 18,6%, к Actinobacteria – 4,1% и к Bacteroidetes – 0,2%. Необходимо отметить, что 2,7% изолятов относились к царству грибов, причем подавляющее большинство (2,47%) – к аскомицетовым дрожжам рода Candida и лишь небольшая часть (0,23 %) – к базидиомицетовым дрожжам рода Rhodotorula. Исследование, проведенное на небольшой группе здоровых добровольцев с использованием молекулярных методов, показало, что наиболее часто встречающимся в ротоглотке типом были бактерии Firmicutes, а видом – S. aureus [9]. Кроме того, авторами выявлено, что на втором и третьем месте по частоте обнаружения были типы Proteobacteria и Bacteroidetes. Согласно данным других исследований, проведенных на смывах со слизистой оболочки глотки у пациентов с ларингеальной карциномой и полипами голосовых связок [8], основными типами являлись Firmicutes (54,7%), Fusobacteria (14,8%), Bacteroidetes (12,7%) и Proteobacteria (10,6%), при этом преобладали бактерии родов Streptococcus spp. (37,3%), Fusobacterium spp. (11,3%), и Prevotella spp. (10,6%). Сравнивая данные литературы с собственными результатами, можно заключить, что основным типом для данного локуса являются Firmicutes, реже встречаются Proteobacteria.
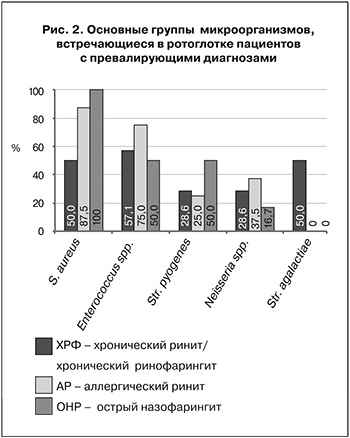 На рис. 2 представлены основные виды/роды бактерий, встречающиеся в ротоглотке пациентов с превалирующими диагнозами. Показано, что S. aureus встречался у всех пациентов при остром назофарингите, несколько реже при аллергическом рините, и только у половины пациентов при хроническом рините/хроническом ринофарингите. По-видимому, эти бактерии являются более характерным микроорганизмом именно для носоглотки. Бактерии Enterococcus spp. и Neisseria spp. чаще всего встречались при аллергическом рините, тогда как Str. agalactiae преобладал у пациентов с острым назофарингитом. Вид Str. pyogenes вообще встречался только у пациентов с хроническим ринитом/хроническим ринофарингитом, что может свидетельствовать о преимущественной принадлежности данного вида бактерий к ротоглотке, нежели к носоглотке.
На рис. 2 представлены основные виды/роды бактерий, встречающиеся в ротоглотке пациентов с превалирующими диагнозами. Показано, что S. aureus встречался у всех пациентов при остром назофарингите, несколько реже при аллергическом рините, и только у половины пациентов при хроническом рините/хроническом ринофарингите. По-видимому, эти бактерии являются более характерным микроорганизмом именно для носоглотки. Бактерии Enterococcus spp. и Neisseria spp. чаще всего встречались при аллергическом рините, тогда как Str. agalactiae преобладал у пациентов с острым назофарингитом. Вид Str. pyogenes вообще встречался только у пациентов с хроническим ринитом/хроническим ринофарингитом, что может свидетельствовать о преимущественной принадлежности данного вида бактерий к ротоглотке, нежели к носоглотке.
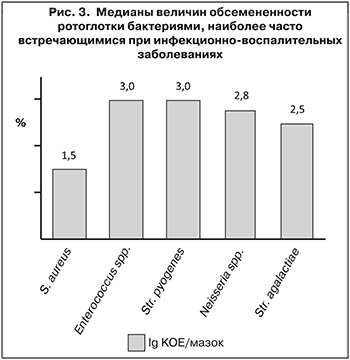
На рис. 3. представлены медианы величин обсемененности ротоглотки наиболее часто встречающимися видами бактерий, оцененные по всему массиву данных. Интересно отметить, что обилие S. aureus, несмотря на его наибольшую среди всех видов бактерий частоту встречаемости, значительно ниже, чем у остальных рассмотренных видов. Лидерами при этом являлись Enterococcus spp. и Str. agalactiae.
Чувствительность полученных изолятов бактерий к ряду антибиотиков определяли диско-диффузионным методом, оценивая при этом процент чувствительных, резистентных (нечувствительных) и умеренно устойчивых штаммов (табл. 2). Обращает на себя внимание относительно низкая чувствительность всех изолятов к аминогликозидам, макролидам и линкозамидам. Рассчитаны коэффициенты корреляции Пирсона (r) для массивов данных о чувствительности микроорганизмов ко всем препаратам в сравнении с соответствующими данными для S. aureus и Enterococcus spp. Видно, что имела место высокая степень корреляции между показателями чувствительности изолятов S. aureus и остальных бактерий (r ≥ 0,9). Примерно та же закономерность обнаружена в отношении умеренно устойчивых штаммов. Однако показатели резистентности штаммов S. aureus и прочих бактерий коррелировали в гораздо меньшей степени (0,5 ≤ r ≤ 0,6). При этом обнаружена высокая степень корреляции между показателями резистентности Enterococcus spp. и Str. agalactiae, Neisseria spp. и Str. pyogenes (r ≥ 0,9), но относительно низкая при сравнении с показателями S. aureus (r = 0,6).
Интересно отметить также, что, суммировав проценты резистентных штаммов к разным антибиотикам для каждого из приведенных видов, можно расположить данные 5 групп микроорганизмов по возрастанию «общей» резистентности в следующей последовательности S. aureus, Str. pyogenes, Neisseria spp., Enterococcus spp., Str. аgalactiae. Допуская, что последние 2 группы являются, скорее всего, наименее патогенными, то есть с высокой частотой встречаются у здоровых людей (энтерококки – до 95% носителей [15], Str. аgalactiae – до 30% [16]), можно рассматривать высокую резистентность их штаммов, выделяемых от здоровых носителей, как положительный фактор. Однако попадание такого штамма от здорового носителя к иммунокомпрометированному лицу может привести к развитию воспаления, которое будет представлять проблему с подбором антибиотика. С этой точки зрения относительно низкая суммарная резистентность S. aureus и Str. pyogenes, высокая условная патогенность которых известна, обнадеживает. Кроме того, имеет место высокая положительная корреляция между показателями (медианами) обсемененности и суммарными показателями резистентности изученных видов (r = 0,853).
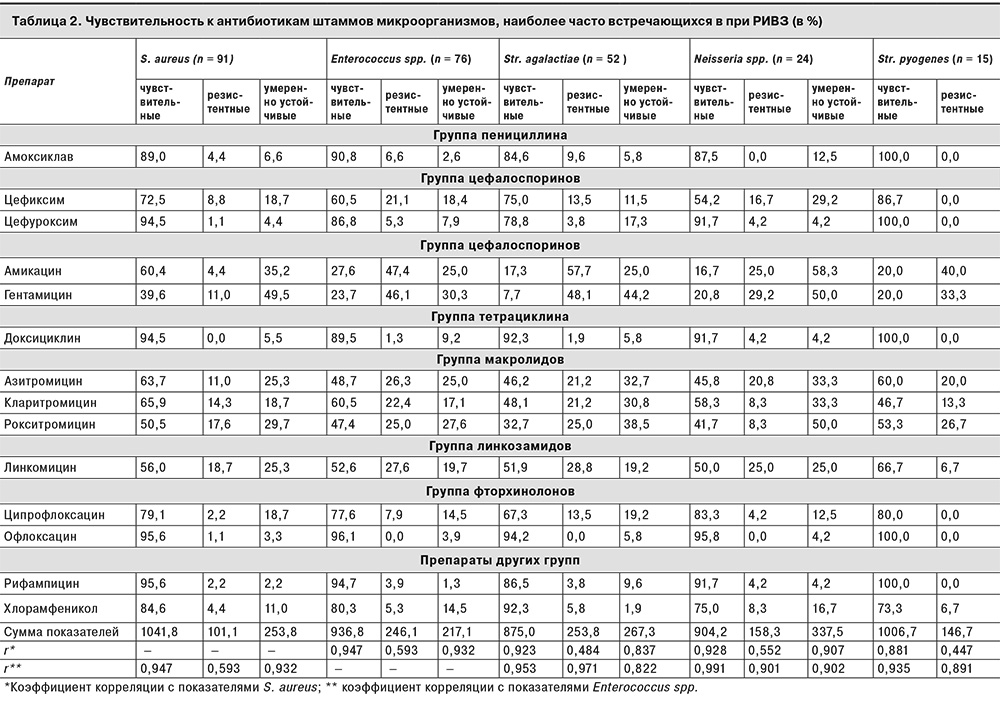
Полученные результаты позволяют заключить следующее: во-первых, очевидно, что S. aureus по своей «общей» резистентности к антибиотикам значительно отличается от прочих рассматриваемых здесь групп микроорганизмов; во-вторых, аминогликозиды, макролиды и линкозамиды имеют невысокую эффективность по сравнению с препаратами других групп, по крайней мере, in vitro, в отношении всех изученных видов бактерий; в-третьих, несмотря на общую типовую принадлежность стафилококков, энтерококков и стрептококков (Firmicutes) и отличную – у нейссерий (Proteobacteria), большее сходство показателей чувствительности (резистентности) проявили микроорганизмы последних 3 групп. Очевидно, обмен информацией, например, в виде плазмид резистентности, происходит не обязательно между более близкородственными бактериями.
 В табл. 3 представлены данные мониторинга чувствительности штаммов S. aureus к некоторым препаратам разных групп: гентамицину (аминогликозид), доксициклину (тетрациклины), азитромицину (аминогликозиды), линкомицину (линкозамиды) и хлорамфениколу (левомицетин). Такой выбор антибиотиков обусловлен тем, что именно эти препараты использовались в клинической практике почти 20 лет назад и используются сейчас.
В табл. 3 представлены данные мониторинга чувствительности штаммов S. aureus к некоторым препаратам разных групп: гентамицину (аминогликозид), доксициклину (тетрациклины), азитромицину (аминогликозиды), линкомицину (линкозамиды) и хлорамфениколу (левомицетин). Такой выбор антибиотиков обусловлен тем, что именно эти препараты использовались в клинической практике почти 20 лет назад и используются сейчас.
Штаммы 1998 и 2005 гг. были выделены с поверхности кожи пациентов с атопическим дерматитом, а 2016 г. – из ротоглотки. Из данных табл. 3 видно, что чувствительность S. aureus к указанным препаратам за прошедшие почти 20 лет менялась, причем неоднозначно. Так, гентамицин постепенно терял активность (снижался процент чувствительных штаммов), однако резистентность к нему за последние 10 лет также снизилась. Остальные препараты, напротив, проявляли самую невысокую активность в 2005 г., а к 2016 г. она значительно возросла, особенно у доксициклина и хлорамфеникола. Наибольший процент штаммов, резистентных к азитромицину, линкомицину и хлорамфениколу, приходился на 2005 г., а к настоящему времени этот показатель значительно снизился. Сравнение динамики изменения чувствительности и резистентности штаммов по трем периодам показало наличие высокой обратной корреляции между этими показателями для всех препаратов, кроме гентамицина. Вероятно, причиной этого является непрерывное и частое применение его в виде пероральных и топических форм на протяжении последних 20 лет. Напротив, остальные препараты широко использовались в более ранний период, затем их популярность снизилась в связи со снижением эффективности, а к настоящему времени их снова целесообразно применять, поскольку доля резистентных к ним форм снова относительно низка.

Выводы
Микробиота ротоглотки является важным клиническим показателем при обследовании пациентов с инфекционно-воспалительными заболеваниями дыхательных путей. На основании результатов посевов из данного локуса и определения чувствительности выявленных условно-патогенных микроорганизмов к антибиотикам врач проводит соответствующую терапию. Настоящее исследование по сути явилось этапом мониторирования видового состава и антибиотикочувствительности микробиоты ротоглотки при РИВЗ.
На наш взгляд, наиболее важными для клиницистов результатами являются следующие:
- Cамыми часто встречающимися видами в данном локусе оказались (в порядке убывания): S. aureus, Enterococcus spp., Str. agalactiae, Neisseria spp., Str. pyogenes.
- Cравнение частоты встречаемости в зависимости от диагноза показало, что S. aureus обнаруживали у всех пациентов при остром назофарингите, реже – при аллергическом рините и только у половины обследованных при хроническом рините/хроническом ринофарингите. Enterococcus и Neisseria чаще всего встречались при аллергическлом рините, тогда как вид Str. agalactiae преобладал у пациентов с острым назофарингитом. Str. pyogenes встречался лишь у пациентов с хроническим ринитом/хроническим ринофарингитом.
- Aминогликозиды, макролиды и линкозамиды проявили невысокую эффективность in vitro по сравнению с препаратами других групп в отношении всех вышеуказанных видов бактерий.
- Чувствительность изолятов S. aureus к гентамицину за 20 лет значительно снизилась, в то время как доксициклин, азитромицин, линкомицин и хлорамфеникол проявляли наименьшую эффективность in vitro в 2005 г., а к настоящему времени этот показатель увеличился.