На протяжении последних 20 лет профилактика вертикальной передачи ВИЧ демонстрирует высокую эффективность метода. По данным ЮНЭЙДС, В 2018 г. количество новых случаев заражения ВИЧ-инфекцией среди детей по сравнению с 2010 г. снизилось на 41% – с 280 000 (190 000–430 000) до 160 000 (110 000–260 000) [1].
Широкий доступ к антиретровирусной терапии (АРТ) и комплексу услуг по профилактике передачи ВИЧ от матери ребенку дал возможность 95–99% детей ВИЧ-позитивных женщин по всему миру рождаться свободными от ВИЧ. Своевременное применение профилактических мер приводит к минимизации числа детей, инфицированных ВИЧ [2–4]. Важной задачей является дальнейшее диспансерное наблюдение, раннее лечение ВИЧ-позитивных и поддержка детей и их матерей для сохранения здоровья и отрицательного ВИЧ-статуса новорожденных, избежавших перинатального заражения. Современная профилактика передачи ВИЧ от матери ребенку – это детально проработанный комплекс мер, в числе которых всеобщий охват АРТ беременных и женщин, планирующих беременность; химиопрофилактика (ХП), проводимая женщине в период родов, новорожденному – после родов; адекватный выбор метода родоразрешения и вскармливания [3–5]. Профилактика проводится на всех этапах возможной передачи вируса в отношении как матери, так и ребенка: беременность и подготовка к ней, роды, послеродовый период. После проведения профилактики во время беременности и родов перед системой здравоохранения встает задача дальнейшего сохранения здоровья детей, рожденных женщинами с ВИЧ, как избежавших инфицирования ВИЧ, так и инфицированных.
По данным литературы, дети ВИЧ-позитивных матерей могут иметь повышенные риски смерти не только в связи с риском ВИЧ-инфицирования, но и из-за недоношенности, сопутствующих заболеваний, особенностей вскармливания, доступности медицинской помощи, что характерно для стран со средним и низким уровнем доходов населения [6, 7]. В развитых странах с высоким доступом к медицинской помощи показатели смертности в когорте детей, рожденных ВИЧ-позитивными женщинами, приближены к общепопуляционным. В целом считается, что при широкой доступности вертикальной профилактики дети, экспонированные по ВИЧ перинатально, имеют сопоставимые показатели смертности с детьми без контакта по ВИЧ, родившихся с одинаковыми показателями здоровья [7, 8].
Постоянный мониторинг профилактики передачи ВИЧ от матери ребенку (ППМР) позволяет оперативно вносить коррективы в существующую практику. Сравнительная оценка показателей смертности детей, рожденных ВИЧ-позитивными женщинами, позволит разработать подходы к профилактике смертности в этой когорте российских детей.
Цель работы – анализ эффективности мероприятий по предотвращению вертикальной передачи ВИЧ в Российской Федерации в 2017–2019 гг. и сравнительная оценка основных показателей детской смертности в России для детей из основной популяции и детей, рожденных от инфицированных ВИЧ матерей.
Материалы и методы
Изучены статистические данные за 2017–2019 гг., находящиеся в свободном доступе: «Основные показатели здоровья матери и ребенка, деятельность службы охраны детства и родовспоможения в Российской Федерации» Минздрава России 2017–2019 гг.»; данные Росстата «Сведения о смертности детей в возрасте до 1 года по причинам смерти в Российской Федерации» за 2018 г.; данные формы мониторинга Роспотребнадзора «Сведения о мероприятиях по профилактике ВИЧ-инфекции, гепатитов В и С, выявлению и лечению больных ВИЧ» за 2017–2019 гг.; формы № 61 государственного статистического наблюдения «Сведения о болезни, вызванной вирусом иммунодефицита человека» Минздрава России за 2017–2019 гг.; данные персонифицированного учета случаев ВИЧ-инфекции ФБУН «Центральный НИИ эпидемиологии» Роспотребнадзора.
Расчет предполагаемого числа детей, инфицированных ВИЧ, проведен с использованием рекомендуемой ВОЗ программы «Spectrum», версия 4, которая позволяет получить оценочные данные и рассчитать уровень передачи ВИЧ от матери ребенку, исходя из объема проведенных профилактических мероприятий, эффективность которых считается установленной более ранними исследованиями.
Расчет показателей смертности проводили по стандартным методикам, рекомендуемым Росстатом.
Результаты
К концу 2019 г. в России число выявленных случаев ВИЧ-инфекции среди женщин превысило 532 000, они составляли 37,4% от всех зарегистрированных больных. Умерли за весь период наблюдения почти 100 000 инфицированных ВИЧ женщин, при этом большинство (70,3%) – в активном трудовом и репродуктивном возрасте (20–40 лет).
По данным Роспотребнадзора, за весь период эпидемии к концу 2019 г. в Российской Федерации было зарегистрировано 301 077 беременностей у ВИЧ-позитивных женщин, из них 206 113 завершились родами. В 2019 г. завершилось родами 13 672 (66,2%) беременности из 20 656 зарегистрированных, а родились живыми 13 714 детей. По данным формы № 61 Минздрава России, за последние 3 года количество родов у женщин с ВИЧ уменьшилось на 8,7%, что отражает общепопуляционные тенденции в РФ, однако число родов остается значительным, а профилактика вертикальной передачи ВИЧ – очень актуальной. 94% ВИЧ-позитивных женщин наблюдались в женской консультации во время беременности, причем этот показатель сопоставим с общей частотой наблюдения беременных в России. Охват профилактическими мероприятиями пар мать–ребенок в 2017–2019 гг. изменился не очень значительно, поскольку уже к 2017 г. были достигнуты высокие значения, но при этом имеется четкая тенденция к продолжению увеличения охвата профилактическими мероприятиями (см. таблицу).

Следует отметить, что в 2019 г. 894 (6,5%) беременные не получили АРТ во время беременности по различным причинам, этот показатель был меньше, чем в 2018 и 2017 гг. – 1102 (7,5%) и 1342 (9,0%) соответственно.
Наименьшего риска передачи ВИЧ от матери ребенку (0,5% и менее) удалось добиться в 2019 г. у детей 5559 (40,7%) женщин, которые начали прием АРТ до беременности, для большинства же беременность оказалась временем старта терапии ВИЧ-инфекции. В предыдущие годы забеременели на фоне АРТ и закончили беременность родами меньше женщин: в 2018 г. – 4654 (31,6%), в 2017 г. – 4004 (26,7%).
Эффективность проводимых мероприятий может быть оценена на основании данных о ВН в период беременности. Особенно важно провести исследование перед родами, когда необходимо планировать интенсивность следующих этапов профилактики во время родов и схему профилактического курса ребенку. Подавляющему большинству беременных было проведено исследование ВН перед родами (см. таблицу).
ВН выше порога определения перед родами в 2019 г. имели 2290 женщин, а также с очень высокой долей вероятности еще 894 женщины, которые не принимали АРТ в период беременности, поскольку у них ВИЧ-инфекция была диагностирована непосредственно перед родами и даже в процессе родов. Таким образом, в 2019 г. было известно о 3184 (23,3%) случаях, когда в связи с определяемой ВН у матери требовалось усиление мер на следующих этапах профилактики (роды и послеродовый период). В 2018 и 2017 гг. таких женщин было 4311 (29,3%) и 3869 (25,8%) соответственно. При этом комбинированную, «усиленную» профилактику, исходя из высокого риска передачи ВИЧ, получили даже несколько больше новорожденных, чем требовалось, исходя из ВН у беременных перед родами: в 2017 г. – 6120 (40,7%), в 2018 г. – 6058 (41,1%), а в 2019 г. – 5396 (39,3%). Вероятно, на практике, «усиленные» схемы профилактики широко назначают новорожденным и в других экстренных случаях, не связанных с ВН матери.
Важно отметить, что 2017–2019 гг. характеризуются высоким охватом ХП вертикальной передачи в родах: в эти годы ее получали 98,7–99,7% детей. При незначительной разнице относительных показателей абсолютное число детей, не охваченных профилактикой, отличается существенно. Так, по данным формы № 61 Минздрава России, профилактика не проведена в 2017 г. 195 (1,3%) новорожденным, в 2018 г. – 132 (0,9%), в 2019 г. таких детей было лишь 45 (0,4%).
По данным Роспотребнадзора, за весь период наблюдения у ВИЧ-позитивных женщин родились 205 675 детей. Наличие ВИЧ-инфекции подтверждено у 11 322 (5,5%), их них 165 детей родились в 2019 г, 220 – в 2018 г. и 273 – в 2017 г. Данные о наличии ВИЧ-инфекции у детей в течение года рождения, согласно форме № 61 Минздрава России, отличались незначительно: 166, 219 и 235 соответственно. Однако в реальности, по данным Роспотребнадзора, ВИЧ-инфекция диагностирована у значительно бóльшего числа новорожденных: в 2019 г. – у 502, в 2018 г. – у 635, в 2017 г. – у 708. Такая значительная разница обусловлена поздней диагностикой ВИЧ-инфекции у детей, родившихся в предыдущие годы. Часто диагноз устанавливают в возрасте 3–6 лет и старше, что сопряжено с риском для жизни и здоровья детей. Раннее установление факта инфицированности позволяет своевременно начать такому ребенку лечение ВИЧ-инфекции и предотвратить тяжелые последствия для здоровья.
Сравнивая расчетное число детей, инфицированных ВИЧ и фактически выявленных, можно определить, какое количество новорожденных остается активно выявить. Например, в 2017 г. расчетный показатель вертикальной передачи ВИЧ составил, согласно методологии программы «Спектрум», 2,3%. Учитывая, что родились всего 15 044 ребенка, диагноз «ВИЧ-инфекция» должен быть установлен у 348 детей, однако фактически в год рождения было выявлено только 67,5% детей от расчетного числа. В 2018 г. тот же показатель составил 2,2%, следовательно, из 14 754 рожденных должно быть выявлено 318 детей, а диагноз выставлен лишь 68,9% из них, что говорит о значительном числе недообследованных или даже умерших детей. Ситуация изменилась в 2019 г., когда уровень вертикальной передачи снизился до 1,8% среди 13 714 рожденных, и расчетное число детей с ВИЧ составило 253. Фактически было выявлено 65,6% детей от расчетного числа. У подавляющего большинства родившихся в 2019 г. детей ВИЧ-инфекция выявлена в ранние сроки, что должно привести к снижению смертности среди них, однако, возможно, у 87 детей диагноз не был выявлен своевременно (не исключено, что в связи со смертью).
В 2017 г. умерли 123 ребенка первого года жизни, 31 (25,2%) из них был инфицирован ВИЧ; в 2018 г. из 132 умерших детей 13 (9,8%) были ВИЧ-инфицированы; в 2019 г. умер 91 ребенок, в том числе 5 (5,5%) детей с диагностированной ВИЧ-инфекцией.
Младенческая смертность в когорте детей, рожденных женщинами с ВИЧ-инфекцией, в 2019 г. составила 6,6 ‰, в 2018 г. – 8,9‰, в 2017 г. – 8,2 ‰. При этом, по данным Росстата, общепопуляционные показатели младенческой смертности были на 26–43% ниже и составили в 2017 г. 5,5‰, 2018 г. – 5,1‰, а в 2019 г. показатель снизился до 4,9%о
Мониторинг причин смерти детей раннего возраста, рожденных женщинами с ВИЧ, затруднен в настоящее время в связи с тем, что информация поступает неполной и со значительным опозданием. Так, данные о детях, родившихся в 2019 г., к маю 2020 г. были ограничены единичными случаями, а из 132 детей, рожденных и умерших в 2018 г., персонифицированная информация была получена только о 94 детях, 6 из которых умерли с диагнозом «ВИЧ-инфекция». В 2018 г. среди ВИЧ-позитивных детей 5 (83,3%) умерли от последствий прогрессии ВИЧ-инфекции, в 1 случае причина смерти не была сообщена. Значительно меньше информации о причине смерти в 2018 г. имелось на 88 детей с отрицательным или неизвестеным ВИЧ-статусом, из них у 51 (58,0%) ребенка отсутствовали сведения о причине смерти. Из 37 случаев с известной причиной смерти в 4 (10,8%) она была указана формально: сердечно-сосудистые заболевания – 2 случая, неврологические заболевания – 1, болезни ЖКТ – 1. Только в 34 случаях были верифицированы причины смерти, часть из которых говорит о том, что умершие дети с высокой долей вероятности были инфицированы ВИЧ. Разделяя причины младенческой смертности по методологии Росстата, можно констатировать, что как причина смерти лидировали инфекционные и пазитарные болезни (сепсис, генерализованная ЦМВИ, генерализованная инфекция, грипп) – 29,4%; болезни органов дыхания (пневмония, туберкулез) – 20,6%. Состояния, возникающие в перинатальном периоде, и врожденные аномалии составили лишь 17,6%, внешние причины (асфиксия, аспирация) – 14,7%, прочие – 17,7%.
По данным общепопуляционного исследования Росстата, у 642 детей, рожденных и умерших в России в 2018 г., основной причиной смерти были состояния, возникающие в перинатальном периоде, и врожденные аномалии – 70,1%, доля инфекционных и паразитарных заболеваний была невелика – 3,4%, болезни органов дыхания составили 3,3%, внешние причины – 6,2%, заболевания ЖКТ – 0,6%, на прочие причины приходилось 16,4%.
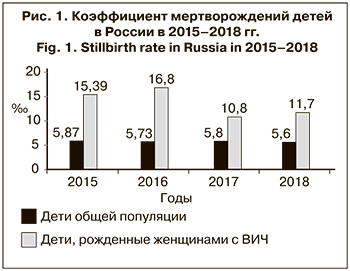 Данные службы охраны детства и родовспоможения показывают, что не только младенческая смертность детей, рожденных ВИЧ-позитивными женщинами, превышает общепопуляционные показатели, но такую тенденцию имеют и все другие показатели, характеризующие смертность детей раннего возраста и акушерско-гинекологическую помощь. Так, в 2018 г. (к моменту написания статьи более поздние сведения были недоступны) коэффициент мертворождений в данной когорте составил 11,7 ‰, тогда как среди общей популяции детей этот показатель был в 2 раза ниже – 5,6 ‰ (рис. 1).
Данные службы охраны детства и родовспоможения показывают, что не только младенческая смертность детей, рожденных ВИЧ-позитивными женщинами, превышает общепопуляционные показатели, но такую тенденцию имеют и все другие показатели, характеризующие смертность детей раннего возраста и акушерско-гинекологическую помощь. Так, в 2018 г. (к моменту написания статьи более поздние сведения были недоступны) коэффициент мертворождений в данной когорте составил 11,7 ‰, тогда как среди общей популяции детей этот показатель был в 2 раза ниже – 5,6 ‰ (рис. 1).
Причем коэффициент мертворождений у женщин с ВИЧ-инфекцией существенно варьировал: от 0 в 31 регионе до 5628‰ в Чеченской Республике, где из 16 родившихся детей, по данным службы охраны детства и родовспоможения, 9 были мертворожденными. Только в Уральском и Сибирском ФО коэффициент мертворождений у женщин с ВИЧ в 2018 г. был ниже среднероссийского и составил 6,9 и 5,8‰ соответственно. В Центральном ФО этот показатель составил 14,2‰, в Северо-Западном – 12,8‰, Южном – 12,6‰, Северо-Кавказском – 62,9‰, Приволжском – 15,7‰, Дальневосточном – 18,8‰. В целом коэффициент мертворождений превышал среднероссийский уровень для когорты детей, рожденных женщинами с ВИЧ, в 35 регионах.
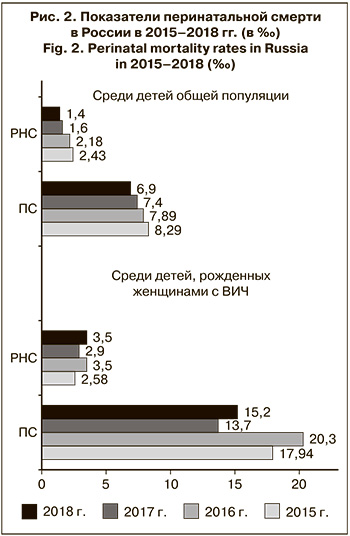 Перинатальная смертность (ПС) в 2018 г. среди детей ВИЧ-позитивных женщин составила 15,2‰, что превосходит общепопуляционный уровень (6,9 ‰) в 2,2 раза. Ожидаемо, что коэффициент ранней неонатальной смерти (РНС – умершие в первые 168 ч/на 1000 родившиеся живыми) среди таких детей также был в 2,5 раза выше общепопуляционного – 3,5 и 1,4‰ соответственно. Соотношение мертворождений и коэффициента РНС составило 3:1. Вызывает озабоченность тот факт, что общепопуляционные показатели, относящиеся к смертности детей раннего возраста, имеют стойкую тенденцию к снижению, тогда как среди детей, рожденных ВИЧ-позитивными женщинами в 2018 г., имеется тренд на повышение (рис. 2).
Перинатальная смертность (ПС) в 2018 г. среди детей ВИЧ-позитивных женщин составила 15,2‰, что превосходит общепопуляционный уровень (6,9 ‰) в 2,2 раза. Ожидаемо, что коэффициент ранней неонатальной смерти (РНС – умершие в первые 168 ч/на 1000 родившиеся живыми) среди таких детей также был в 2,5 раза выше общепопуляционного – 3,5 и 1,4‰ соответственно. Соотношение мертворождений и коэффициента РНС составило 3:1. Вызывает озабоченность тот факт, что общепопуляционные показатели, относящиеся к смертности детей раннего возраста, имеют стойкую тенденцию к снижению, тогда как среди детей, рожденных ВИЧ-позитивными женщинами в 2018 г., имеется тренд на повышение (рис. 2).
Обсуждение
В последние годы отмечается устойчивое, хотя и медленное расширение охвата АРТ ВИЧ-позитивных беременных, однако в 2017–2019 гг. 12,8–8,5% из них не принимали АРТ до родов по различным причинам.
Большинство ВИЧ-позитивных беременных наблюдаются в связи с ВИЧ-инфекцией и для них нет необходимости в активном привлечении к диспансерному наблюдению и лечению, а оставшиеся требуют особого подхода, программ лечения «низкого доступа», так как имеют поведенческие и социальные особенности (женщины-наркопотребители, мигранты и другие труднодоступные группы). Изучение и работа с факторами, приводящими к отсутствию приема антиретровирусных препаратов, является ресурсом повышения эффективности вертикальной профилактики.
В 2019 г. по сравнению с 2017–2018 гг. у значительно бóльшего числа женщин наступила беременность на фоне контролируемой АРТ, однако большинство беременных начали прием АРТ в период беременности, что говорит, с одной стороны, о высокой частоте новых случаев ВИЧ-инфекции в этой когорте, с другой – о недостаточном охвате АРТ молодых ВИЧ-позитивных женщин.
Отмечается широкий охват беременных обследованием на ВН, которое позволяет оценить эффективность проводимой профилактики, вовремя ее скорректировать и выбрать метод ведения родов с учетом снижения риска передачи ВИЧ ребенку. Пожалуй, наиболее актуальной задачей можно считать повышение приверженности беременных наблюдению и лечению, так как у значительного числа женщин ВН остается определяемой, несмотря на проводимую профилактику. Согласно официальным данным Минздрава России, в 2019 г. у 18,2% женщин перед родами ВН была выше порога определения, что может быть следствием как позднего начала АРТ, так и неприверженности лечению женщин, вовремя начавших терапию. В любом случае эффективность приема АРТ во время беременности у таких женщин находится под сомнением. А если суммировать эту долю с долей женщин, вообще не принимавшими АРТ, можно заключить, что для значительного числа детей (3184) риск вертикальной передачи ВИЧ не был минимальным. В 2017–2019 гг. таких детей было еще больше. В 2019 г. снизилось число новорожденных, получающих усиленные схемы ХП. Сопоставляя эти данные с увеличением в 2019 г. числа женщин, начавших принимать АРТ до беременности, несколько большим охватом ХП беременных, можно предположить, что снижение доли усиленных схем ХП у новорожденных связано с меньшей вероятностью ситуаций, требующих экстренных мер.
Отдельной, малоизученной и, вероятно, весьма чувствительной темой является смертность детей, рожденных женщинами с ВИЧ. При этом тема смертности детей раннего возраста в целом является приоритетом здравоохранения. Снижение младенческой смертности – одна из основных целей национального проекта «Здравоохранение». К 2025 г. смертность детей первого года жизни планируется снизить до 4,5 случая на 1000 родившихся живыми [9]. В когорте детей, рожденных ВИЧ-позитивными женщинами, этот показатель превышает среднероссийский в 1,3 раза. При этом в структуре смертности детей в общей популяции преобладают «состояния, возникающие в перинатальном периоде и врожденные аномалии», что является общемировым трендом при доступной и качественной медицинской помощи. Среди детей ВИЧ-позитивных женщин наблюдается другая картина: преобладают «инфекционные заболевания», существенную роль играют болезни органов дыхания, внешние причины (асфиксия, аспирация), а «состояния, возникающие в перинатальном периоде и врожденные аномалии» играют второстепенную роль. Дети, умершие с известным ВИЧ-позитивным статусом, чаще имели верифицированный посмертный диагноз, указанную конкретную причину смерти. У детей с неопределенным ВИЧ-статусом, среди которых с высокой долей вероятности имелись ВИЧ-позитивные, причина смерти часто не верифицируется или остается неизвестной службе центров СПИДа, осуществляющих диспансерное наблюдение и лечение при ВИЧ-инфекции. Следует отметить, что в 2019 г. существенно снизить младенческую смертность детей, рожденных ВИЧ-позитивными женщинами, удалось, вероятно, за счет сокращения числа смертей новорожденных с ВИЧ-инфекцией из-за расширения охвата ранней диагностикой ВИЧ-инфекции и быстрого назначения лечения детям первых месяцев жизни.
Однако беспокоят высокие цифры перинатальной смертности, коэффициента мертворождения, младенческой смертности в когорте детей, рожденных ВИЧ-позитивными матерями, по сравнению с общепопуляционным уровнем. Высокая доля как инфекционных заболеваний, так и «состояний, возникающих в перинатальном периоде и врожденных аномалий» в структуре причин летальных исходов говорит о вероятном существенном значении внутриутробных инфекций (ВУИ или «инфекций перинатального периода»), роль которых в структуре ранней смертности детей, затронутых проблемой ВИЧ-инфекцией, совершенно не изучена. Этот вопрос становится крайне актуальным в связи с успехами профилактики вертикальной передачи ВИЧ-инфекции. Можно констатировать, что среди умерших детей в возрасте до 1 года, матери которых ВИЧ-позитивны, не все заражены ВИЧ.
Вероятно, существующие программы скрининга беременных и детей на инфекционные заболевания, оказывающие влияние на жизнь и здоровье новорожденных в изучаемой когорте, не так эффективны, как хотелось бы специалистам. Спектр антенатальной и интранатальной инфекционной патологии не ограничивается вирусными гепатитами, сифилисом, краснухой, а включает инфекции, вызванные цитомегаловирусом (ЦМВ), вирусом простого герпеса (ВПГ) 1-го и 2-го типов, вирусом Varicella zoster, токсоплазмами, листериями. Частота врожденных инфекционных заболеваний при наличии ВИЧ у беременной существенно выше. Так, если в общей популяции ЦМВ-инфекцию (ЦМВИ) у живых новорожденных диагностируют в 0,2–2,5% случаев, то у детей, рожденных ВИЧ-позитивными матерями, – до 6,9% [10–13]. По тератогенной значимости ЦМВ занимает второе место после вируса краснухи, это также основная причина врожденной патологии ЦНС, врожденных пороков, задержки психического и умственного развития у детей раннего возраста, не имеющих хромосомных нарушений, и главная причина врожденной сенсоневральной потери слуха. Около 20–30% детей с манифестной ЦМВИ погибают в первые годы жизни (2/3 – в первые 12 мес. жизни), у 90% выживших развиваются поздние неврологические осложнения [11, 12, 14]. Если ребенок, зараженный ЦМВ, токсоплазмами, ВПГ во время внутриутробного развития или родов, останется не инфицированным ВИЧ благодаря отлаженной системе профилактики вертикальной передачи ВИЧ, но будет страдать серьезной неврологической и психической патологией – можно ли говорить о высоком качестве и большой продолжительности его «не ВИЧ-инфицированной» жизни? Следует признать, что сегодня в области акушерства и неонатологии (в том числе при ведении ВИЧ-инфицированных беременных и их детей) отсутствуют современные регламентирующие документы по проблеме каждой из внутриутробных инфекций, отсутствует консенсус между акушерами-гинекологами, неонатологами, детскими реаниматологами и инфекционистами по методам диагностики, лечения, ведения в целом беременных с острыми или вторичными активными инфекциями, а также новорожденных, анте- или интранально зараженных теми или иными возбудителями ВУИ.
Таким образом, структура смертности говорит о недостаточном охвате необходимыми видами обследования инфицированных ВИЧ беременных и новорожденных, дефиците педиатрического и социального патронажа семей с маленькими детьми указанной категории, низком качестве и доступности медицинской помощи детям, рожденным ВИЧ-позитивными женщинами. Если ставить целью снижение показателей перинатальной смертности, коэффициента мертворождения, младенческой смертности детей, рожденных ВИЧ-инфицированными матерями, обеспечение здоровья детям, матери которых ВИЧ-позитивны, необходимо думать не только о профилактике вертикальной передачи ВИЧ, вируса гепатита В, сифилиса, но и возбудителей других инфекций перинатального периода (ЦМВ, ВПГ, вируса Varicella zoster, токсоплазмоза). Необходимо включить в рекомендации и протоколы ведения ВИЧ-положительных беременных и их детей алгоритмы диагностики и лечения целого ряда внутриутробных инфекций.
Выводы
Исследование показало высокий охват беременных и новорожденных ХП передачи ВИЧ-инфекции от матери ребенку в Российской Федерации в последние 3 года.
Среди актуальных направлений профилактики вертикальной передачи ВИЧ можно выделить:
- расширение охвата лечением ВИЧ-позитивных женщин детородного возраста;
- широкое внедрение мер по работе с беременными женщинами, относящимся к группам риска;
- особое внимание следует уделить приверженности беременных наблюдению и лечению, инструментами которой являются консультирование, работа мультипрофессиональной команды специалистов.
В когорте детей, рожденных ВИЧ-позитивными женщинами, показатели смертности остаются высокими в сравнении с общепопуляционным уровнем. Необходимо дальнейшее выявление факторов, влияющих на повышенную смертность детей раннего возраста, а также разработка и внедрение мер профилактики повышенного риска перинатальной и младенческой смерти, среди которых ведущее место занимают современная диагностика и лечение актуального спектра внутриутробных инфекций.