Менингококковая инфекция (МИ) остается смертельно опасным инфекционным заболеванием, отличающимся внезапностью развития, тяжестью течения и риском неблагоприятных исходов [1, 2]. Особенностью МИ является цикличность эпидемического процесса с периодическими подъемами заболеваемости через 8–30 лет. По данным экспертов, очередное начало подъема заболеваемости МИ прогнозируется в 2019–2025 гг. [3–5]. Обзор современной литературы [6–9] показывает, что повсеместная циркуляция возбудителя в виде бессимптомного носительства, воздушно-капельный путь передачи инфекции, серогрупповое разнообразие возбудителя и миграционные потоки лежат в основе периодической активизации эпидемического процесса МИ, что требует неотлагательного решения вопросов специфической профилактики МИ в соответствии с требованиями ВОЗ [10].
В последние годы появляются данные о случаях атипичного течения МИ [11]. Клинический полиморфизм генерализованных форм МИ (ГФМИ), отсутствие патогномоничных признаков в первые часы болезни определяют трудности ранней диагностики, что в ряде случаев является причиной поздней госпитализации, развития осложнений и неэффективности реанимационных мероприятий [12]. Однако несмотря на острое и иногда молниеносное течение заболевания, в большинстве случаев знание клинико-эпидемиологических особенностей МИ на современном этапе позволяет своевременно диагностировать инфекцию, правильно определить тактику неотложных мероприятий, и тем самым снизить риски развития неблагоприятного исхода.
Цель нашего исследования – изучение клинико-эпидемиологических особенностей МИ у больных в Республике Узбекистан.
Материалы и методы
Проведенo проспективное исследование эпидемиологических и клинико-лабораторных данных 118 пациентов в возрасте от 6 мес. до 65 лет с ГФМИ, находившихся на лечении в Городской клинической инфекционной больнице № 1 г. Ташкента в период с января по май 2019 г. Все больные поступали в тяжелом состоянии в отделение реанимации и интенсивной терапии, по мере улучшения состояния их переводили в менингитное отделение для продолжения лечения. У всех поступивших больных брали мазок из носоглотки, при выявлении менингеальных симптомов проводили люмбальную пункцию. Ликвор отправляли в лабораторию для биохимического и микробиологического анализов. Диагноз МИ устанавливали на основании совокупности патогномоничных клинических симптомов (острейшее начало заболевания, стойкая гипертермия, наличие характерной геморрагической сыпи), менингеальных симптомов, эпидемиологических и лабораторных данных.
Динамическое наблюдение за больными проводили на протяжении всего периода пребывания в стационаре. Средняя продолжительность стационарного лечения составила 15 ± 4,1 дня. Клиническое наблюдение дополняли общеклиническими лабораторными исследованиями (общий анализ крови, мочи, кала), бактериологическим исследованием крови и ликвора. Биохимические исследования крови, рентген, МРТ проводили по клиническим показаниям. Всех больных, в материалах которых выделяли N. meningitidis, вне зависимости от возраста включали в базу для последующего анализа.
У всех больных исследовали гемокультуры. Забор крови (в соотношении 1:10) проводили из двух рук до начала антимикробной терапии во флаконы (HiCombi, двухфазная система для гемокультур производства компании Himedia, Индия). Засеянные флаконы инкубировали в термостате и отмечали появление мутности, изменение цвета среды, гемолиза и/или газообразования с последующим посевом на шоколадный и кровяной агар, с дальнейшей идентификацией на основе морфологии колоний, окрашивания по Граму, результатлов каталазной и оксидазной реакций. Все изоляты были исследованы на чувствительность к противомикробным препаратам в соответствии с рекомендациями и стандартами EUCAST (2018). Определяли серогруппы выделенных от больных штаммов Neisseria meningitidis методом латекс-агглютинации с использованием набора Wellcogen на менингококковые инфекции Wellcogen Bacterial Antigen Kit.
По результатам исследования была сформирована база данных, на основе которой с помощью пакета прикладных программ Microsoft Office 2017 Proffessional STATISTICA 6.1 осуществлялся статистический анализ.
Результаты
По официальным данным Республиканского центра государственного санитарно-эпидемиологического надзора Министерства здравоохранения Республики Узбекистан, в последние годы заболеваемость МИ в стране сохранялась в пределах 0,3 – 0,2 на 100 тыс. населения, однако с января 2019 г. отмечено резкое повышение заболеваемости: за период с января по май зарегистрировано 123 случая заболевания ГФМИ (рис. 1). ГФМИ характеризуются не только тяжестью течения, но и возможностью летального исхода и значительной частотой осложнений заболевания с последующей инвалидизацией [13]. Несмотря на наличие специфических опорно-диагностических признаков, современные особенности течения этого заболевания как у детей, так и у взрослых могут стать возможной причиной диагностических, тактических и лечебных ошибок на разных этапах оказания медицинской помощи, способствующих развитию неблагоприятных исходов болезни.

Процент бактериологического подтверждения этиологии МИ колеблется, по данным разных авторов, от 6 до 70% в зависимости от оснащенности лабораторий [1, 2]. Низкий процент бактериологического подтверждения этиологии заболевания и получение результата не в 1-е сутки с момента исследования показывает необходимость расширения объема проводимых лабораторных исследований с использованием методов экспресс-диагностики.
Анализ возрастной структуры пациентов с ГФМИ показал, что высокая заболеваемость отмечена среди взрослых в возрасте 20–29 лет (39,8%) и детей 7–14 лет (17,9%) (рис. 2).
92 (78%) больных были жителями Ташкента, остальные 26 (22%) – приезжие из разных областей Узбекистана. Более чем в 50% случаев имел место семейный контакт, когда из одной семьи поступали несколько детей, иногда вместе с родителями.
Сезонный анализ заболеваемости ГФМИ показал, что более половины больных были госпитализированы в марте. В январе и феврале регистрировались единичные случаи МИ, а обратившиеся за медицинской помощью были гражданами Узбекистана, проживающими в Ташкенте, приехавшими накануне из соседних стран (в том числе из России), иногда уже с признаками инфекции. С конца февраля и в марте число заболевших резко увеличилось и среди контактных лиц. С мая отмечено снижение числа госпитализаций, что, возможно, связано с быстрым реагированием санитарно-эпидемиологической службы, проведением профилактических и противоэпидемических мероприятий, в частности, выявлением контактных лиц, изоляцией лиц с локализованной формой МИ (назофарингитом), вакцинацией и химиопрофилактикой в группах риска и среди контактных лиц.
 Социально-профессиональный состав заболевших МИ был представлен рабочими-строителями (27/22,8%), школьниками (33/27,9%), студентами (15/12,7%) и др.
Социально-профессиональный состав заболевших МИ был представлен рабочими-строителями (27/22,8%), школьниками (33/27,9%), студентами (15/12,7%) и др.
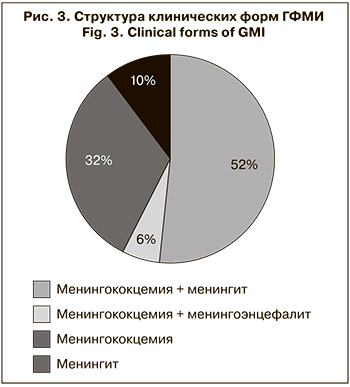
Среди клинических форм ГФМИ основной остается смешанная форма, установленная у 68 (57,6%) больных. При этом следует отметить, что разные клинические формы равномерно встречались во всех возрастных группах (рис. 3).
У всех больных имел место типичный классический вариант развития болезни. Острое начало характеризовалась повышением температуры тела до 39,5–40 °С с первых часов болезни. Особенностью гипертермии является ее устойчивость к назначению жаропонижающих средств, даже при снижении на 1–2 °С через некоторое время она вновь достигает высоких цифр. У детей гипертермия сопровождалась изменением поведения и нарушением сна, выраженным психомоторным возбуждением (12/10,6%), причем наиболее часто оно имело место у детей первого года жизни. У большинства больных развивались вялость и адинамия, которые у детей в возрасте до 3 лет встречались в 100% случаев. У 78 (64,4%) больных в начале заболевания появлялась рвота, которая в ряде случаев была многократной. С первых часов болезни у 86 (72,8%) пациентов отмечалась резкая гиперестезия ко всем видам раздражителей, у детей это проявлялось чувствительностью к свету, любым прикосновениям. Особенностью интоксикационного процесса у детей в возрасте до 3 лет являлся пронзительный монотонный плач. Интенсивную головную боль диффузного распирающего характера, усиливающуюся при изменении положения тела, регистрировали в 72 (61,0%) случаях, чаще у больных старшего возраста. 13 (11,0%) больных отмечали потерю сознания. На фоне дегидратирующей терапии через 2–3 дня головная боль уменьшалась и к 4–5-му дню болезни исчезала.
Патогномоничным симптомом менингококцемии и сочетанных вариантов ГФМИ является геморрагически-некротическая сыпь звездчатой формы. У подавляющего большинства больных (96,6%), находившихся под нашим наблюдением, сыпь появлялась в 1-е сутки заболевания, чаще после 12 ч от начала болезни; на 2-й день высыпания увеличивались. Раннее появление сыпи (в первые 5–8 ч) было характерно для тяжелых гипертоксических форм МИ, оно отмечено у 5 (4,2%) детей в возрасте до 3 лет и у 3 (2,2%) детей в возрасте 4–7 лет. Сыпь была геморрагически-некротической и пятнисто-папулезной, звездчатой формы, располагалась на всех участках тела, но у 83 (70,3%) была локализована на нижних конечностях и нижней части туловища. При ГФМИ, сопровождающейся развитием инфекционно-токсического шока (ИТШ) II–III степени, высыпания вначале появлялись на лице и верхней части туловища, а затем распространялись на конечности. Пятнисто-папулезная сыпь была характерна для больных старшего возраста, и именно эти случаи представляли для врачей скорой помощи и врачей общей практики трудность в распознавании МИ на догоспитальном этапе. Только на 3–4-е сутки заболевания на фоне сохраняющейся фебрильной лихорадки возникали классические геморрагически-некротические высыпания с одновременным развитием ИТШ, что значительно затрудняло своевременную постановку диагноза. По-прежнему наиболее частым ранним осложнением ГФМИ является ИТШ: его проявления были отмечены у 72 (61,0%) больных. Превалировал ИТШ I степени, его регистрировали у 46 (63,8%) больных. Реже встречался ИТШ II и III степени – у 20 (27,7%) и 6 (8,3%) больных соответственно.
Менингококковый менингит наблюдали у 12 (10,2%) больных. Он характеризовался острым началом; повышением температуры тела; интоксикацией; головными болями распирающего характера; гиперестезией; рвотой, не приносящей облегчения; положительными менингеальными симптомами (ригидность затылочных мышц, симптомы Брудзинского и Кернига); гнойным характером ликвора.
Важнейшим фактором риска неблагоприятного исхода заболевания являлся возраст больного (дети до 1 года), а также позднее обращение за медицинской помощью. Выявлено, что в 63 (53,3%) случаях больные обращались за медицинской помощью в первые 12 ч от начала заболевания, в 55 (46,7%) – на 2-е сутки болезни. Однако анализ сроков госпитализации показал, что 52% больных были госпитализированы при первом обращении, 36% – при повторном вызове бригады скорой помощи, а в 12% случаев больные были госпитализированы после повторных вызовов и осмотров врачами скорой помощи или врачами общей практики.
Исходы ГФМИ отличаются развитием тяжелых резидуальных нарушений, которые могут в дальнейшем не только снизить качество жизни, но и привести к инвалидизации. Чаще всего у наблюдаемых больных регистрировали гипертензионно-гидроцефальный синдром, для которого характерны головная боль диффузного характера, периодические головокружения, снижение памяти, внимательности, быстрая утомляемость, а также нейросенсорная тугоухость (3,3%), лобно-мозжечковая атаксия (5%), резидуальная энцефалопатия (11,8%), симптоматическая эпилепсия (3,3%). Эти больные состоят на диспансерном учете и регулярно посещают невролога. При тяжелых вариантах менингококцемии развивались глубокие некрозы, которые формируют в дальнейшем кожные рубцы и требуют повторных пластических операций [2].
Результаты исследования серогрупповой принадлежности штаммов N. meningitidis, выделенных от больных с ГФМИ, показали, что начиная с периода подъема заболеваемости, в лабораторно подтвержденных случаях заболевания основным возбудителем является N. meningitidis серогруппы А (99,1%) (рис. 4).
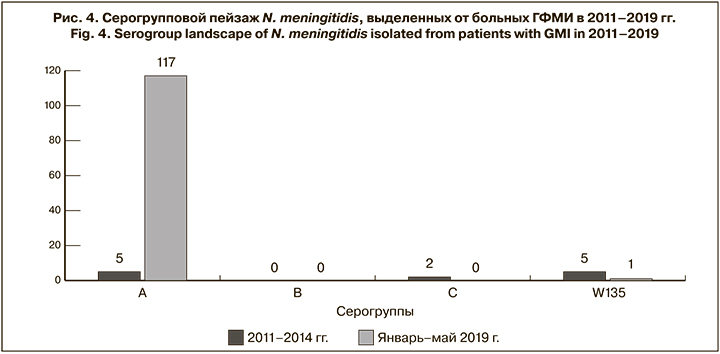
Необходимо помнить, что этиологическая диагностика с определением серогрупповой принадлежности N. meningitidis является неотъемлемой частью эпиднадзора за МИ. Его цель – оценка эпидемической ситуации, составление прогноза на ближайшие годы и разработка рекомендаций по проведению профилактических мер для снижения заболеваемости и летальности. С учетом эпидемической ситуации по МИ, сложившейся в начале 2019 г., для снижения дальнейшего распространения МИ среди населения были выявлены и вакцинированы все контактные с лица, что привело к резкому снижению заболеваемости МИ в Узбекистане в июне 2019 г.
Обсуждение
Обзор опубликованных источников литературы и результаты наших наблюдений показывают, что в современных условиях в Республике Узбекистан меняется структура ГФМИ. Так, по данным Р.И. Касымова (2008), в предыдущие годы отмечались преимущественно изолированные формы МИ в виде менингококкового менингита, тогда как по нашим наболюдениям увеличилась частота комбинированной формы: менингококцемия + менингит, а также уменьшилась доля изолированного менингита в структуре клинических форм заболевания. Классическое течение МИ с острым началом, проявлениями высокой интоксикации, геморрагической сыпью звездчатой формы до сих пор остается основой для клинической диагностики ГФМИ. Наши наблюдения показали, что встречаются клинические формы, когда геморрагическая сыпь на фоне стойкой гипертермии появляется только на 3–4-е сутки заболевания, что значительно затрудняет своевременную постановку диагноза.
По данным литературы [2, 3, 7], на сегодняшний день в большинстве случаев ответственными за развитие ГФМИ являются менингококки серогруппы W135. Результаты нашего исследования показали, что начиная с периода подъема заболеваемости (январь 2019 г.) лидирующей является серогруппа А (99,1%), и только в 1 (0,9%) случае была определена N. meningitidis серогруппы W135 (0,9%).
Нужно отметить, что заболеваемость МИ в мире в течение последнего десятилетия регистрируется на постоянном уровне, а ее периодические подъемы связывают со сменой ведущей серогруппы возбудителя, вызывающего ГФМИ, и снижением коллективного иммунитета. При этом сохраняется высокая (до 15%) летальность, обусловленная как тяжестью патологического процесса, так и отдельными ошибками клинической диагностики, несвоевременной госпитализацией и сроками начала адекватного комплексного лечения. Кроме этого, внимание к МИ вызвано распространенностью ее во всем мире за счет выраженной миграции, путешествий и паломничества, что определяет генетическую изменчивость возбудителя и необходимость разработки адекватной специфической профилактики.
В настоящее время с учетом эпидемической ситуации в мире, внедрение вакцинации против МИ в календари профилактических прививок является весьма актуальной. Для предупреждения МИ применяются вакцины нескольких типов: полисахаридные моно- и поливалентные вакцины серогрупп A, C, W135 и Y; конъюгированные моновакцины (против менингококков серогрупп С и А), конъюгированные четырехвалентные (ACWY). В Узбекистане вакцинация против МИ не включена в национальный календарь профилактических прививок. Иммунизации против МИ подлежат лица, контактные с больными МИ, а также проводится плановая иммунизация военнослужащих. Таким образом, в связи с эпидемическим подъемом заболеваемости МИ на территории Узбекистана в 2019 г., а также ожидаемым дальнейшим ростом заболеваемости МИ во всем мире, вопросы, касающиеся ранней диагностики, лечения и специфической профилактики МИ являются весьма актуальными и требуют повышения уровня систематического эпидемического надзора как в Республике Узбекистан, так и в других странах.
Выводы
- Эпидемическая ситуация по МИ в Узбекистане имеет признаки межэпидемического периода.
- В возрастной структуре больных высок удельный вес детей в возрасте 7–14 лет (17,9%) и взрослых 20–29 лет (39,8%).
- В лабораторно подтвержденных случаях МИ лидирующим возбудителем является N. meningitidis серогруппы A (99,1%), при этом в предыдущие годы были отмечены случаи заболевания, вызванного N. meningitidis серогрупп W135 и С.
- Наблюдаются клинические формы ГФМИ, при которых характерная геморрагическая сыпь на фоне стойкой гипертермии появляется только на 3–4-е сутки заболевания, что значительно затрудняет своевременную постановку диагноза.
- У реконвалесцентов, перенесших комбинированную форму МИ и «чистый» менингит, возможно развитие тяжелых резидуальных последствий, приводящих к инвалидизации: нейросенсорной тугоухости (3,3%) и резидуальной энцефалопатии (11,8%). Возможно также развитие глубоких некрозов с образованием рубцов на месте высыпаний.
- Снизить заболеваемость и смертность от ГФМИ среди детей и взрослых позволит использование поливалентных конъюгированных вакцин против МИ в потенциальных группах риска.