Снижение репродуктивного потенциала населения – одна из главных проблем здравоохранения развитых стран. Изучение причин нарушения репродуктивного здоровья в настоящее время является одним из основных направлений развития медицинской науки в России. Концепция демографической политики Российской Федерации на период до 2025 г., утвержденная Указом Президента № 1351 от 9 октября 2007 г., определила укрепление репродуктивного здоровья и института семьи в качестве приоритетных направлений государственной политики, так как от них зависит не только уровень рождаемости, но и жизнеспособность следующих поколений1. В связи с этим лица в возрасте от 15 до 39 лет – та социально значимая группа, состояние здоровья которой будет определять демографическую ситуацию в будущем.
Причины, оказывающие негативное влияние на репродуктивное здоровье населения, многообразны. К заболеваниям, приводящим к нарушению репродуктивного здоровья, относятся и злокачественные новообразования (ЗНО), которые занимают 2-е место в мире в общей структуре причин смертности, уступая только сердечно-сосудистым болезням [1]. Вероятность наступления беременности у пациенток, перенесших онкологическое заболевание, на 67% ниже, чем в общей популяции [2]. Репродуктивные проблемы после перенесенных онкологических заболеваний включают опасения не только по поводу фертильности, но и по поводу факторов, связанных с качеством жизни, возможностью воспитания детей, генетической предрасположенностью к раку у детей и т. д. [3].
Значимость таких заболеваний, с одной стороны, обусловлена увеличением числа пациентов, высоким риском летального исхода или развития нежелательных эффектов во время лечения; с другой – изучением новых методов диагностики и расширением возможности терапии, что позволяет сохранить жизнь и здоровье пациентов [4].
Несмотря на ежегодное увеличение количества исследований, посвященных изучению ЗНО у подростков и молодых взрослых, знаний о причинах и эпидемиологических тенденциях недостаточно [5]. Также следует подчеркнуть важность дифференциации показателей по полу и возрасту, поскольку распределение ЗНО среди подростков и молодых людей существенно отличается от такового у детей и пожилых лиц [6, 7].
Цель исследования – анализ заболеваемости и смертности от ЗНО органов репродуктивной системы мужчин и женщин в возрасте от 15 до 39 лет за 2008–2020 гг. в Российской Федерации.
Материалы и методы
В исследование были включены все зарегистрированные случаи ЗНО органов репродуктивной системы: рак молочной железы, предстательной железы, мочевого пузыря, вульвы, влагалища, шейки и тела матки, яичников, плаценты, полового члена и яичка, диагностированные у лиц от 15 до 39 лет за 2008–2020 гг. в Российской Федерации. Использовался диапазон от 15 до 39 лет, поскольку это рекомендованное определение возрастного диапазона лиц основного репродуктивного возраста в онкологии [8]. Расчеты были проведены в соответствии с информацией специализированных форм государственной отчетности № 7 «Сведения о заболеваниях злокачественными новообразованиями» и № 35 «Сведения о больных со злокачественными новообразованиями», статистическими сведениями (половозрастной состав населения территорий) Федеральной службы государственной статистики. Оценивали следующие показатели, характеризующие эпидемическую ситуацию: заболеваемость и смертность с 95% доверительными интервалами (ДИ) и среднегодовой темп прироста по 11 видам рака, которые были включены в исследование. Интенсивные эпидемиологические показатели рассчитывали на 100 000 населения соответствующих возрастно-половых групп. Анализ и обработка данных проведены с помощью программы Microsoft Office Excel 2010.
Результаты
В целом за 2008–2020 гг. в Российской Федерации было зарегистрировано 135 824 заболеваний и 27 776 смертей от ЗНО репродуктивных органов среди возрастной группы подростков и молодых людей. В 2021 г. зарегистрировано 556 036 новых случаев ЗНО, из которых 26 609 – у лиц в возрасте от 15 до 39 лет, среди них 10 643 (40%) случаев ЗНО органов репродуктивной системы [9].
Расчетный показатель заболеваемости ЗНО репродуктивных органов в РФ среди населения 15–39 лет обоих полов значительно увеличился с 15,5 (95% ДИ 15,2–15,8) на 100 тыс. населения в 2008 г. до 23,8 (95% ДИ 23,3–24,2) в 2019 г. (среднегодовой темп прироста +3,7%), в 2020 г. показатель снизился до 22,3 на 100 тыс. населения.
Данный показатель в Москве вырос с 12,6 до 18,8 на 100 тыс. населения в 2019 г. (среднегодовой темп прироста +3,7%) и снизился до 16,4 на 100 тыс. населения в 2020 г.
Наиболее интенсивно растет заболеваемость в возрастной подгруппе 30–39 лет, в которой показатель находился на уровне 37,4 (95% ДИ 36,6–38,2) на 100 000 тыс. населения, что составило 86,5% всех случаев в группе 15–39 лет в 2020 г., тогда как в группе 15–19 лет отмечен показатель 1,7 (95% ДИ 1,4–2,0) случая на 100 тыс. населения, его доля составила 1,1%. Рост заболеваемости отмечен во всех возрастных группах. Среднегодовой темп прироста с 2008 по 2020 г. среди лиц 15–19 лет составил +2,4%, 20–29 лет – +1,4%, 30–39 лет – +1,6% (рис. 1, а).
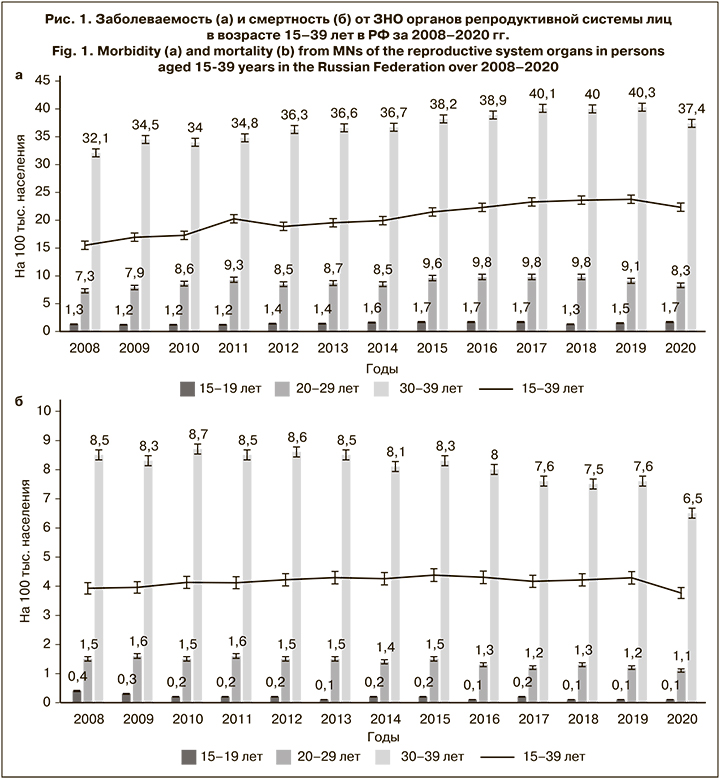
Показатель смертности сохраняется примерно на одном уровне, без выраженных тенденций к снижению или росту на протяжении всего изучаемого периода – 3,9 (95% ДИ 3,8–4,1) на 100 тыс. населения в 2008 г. и 4,3 (95% ДИ 4,1–4,5) в 2019 г. (среднегодовой темп прироста – +0,3%). В 2020 г. показатель составил 3,8 на 100 тыс. населения (рис. 1, б).
В РФ у женщин с выявленными ЗНО репродуктивных органов в возрасте от 15 до 19 лет превалирует рак яичников (1,5 на 100 тыс. в 2020 г.), в возрастной группе 20–29 лет лидирующую позицию занимают новообразования шейки матки (5,1 на 100 тыс. в 2020 г.), а в возрасте 30–39 лет на 1-е место совместно с новообразованиями шейки матки (14,5 на 100 тыс. в 2020 г.) выходят новообразования молочных желез (18,2 на 100 тыс. в 2020 г.). У мужчин на всем возрастном промежутке от 15 до 39 лет самым распространенным среди репродуктивных новообразованием остается рак яичка (3,3 на 100 тыс. в 2020 г.) (рис. 2).

В структуре заболеваемости ЗНО репродуктивных органов лиц молодого возраста наибольшая доля приходится на новообразования молочных желез (16,1%), шейки матки (12,8%) и яичников (4,1%).
Структура заболеваемости меняется в зависимости от возраста. Среди женщин 15–19 лет 1-е место занимает рак яичников (74%), 2-е – рак шейки матки (РШМ; 8,7%), 3-е – рак молочной железы (4,7%). У женщин в возрасте 20–29 лет 1-е место занимает РШМ (44,7%), далее следуют рак молочной железы (23,1%) и рак яичников (23,0%). Среди женщин 30–39 лет 1-е место занимает рак молочной железы (41,3%), 2-е – РШМ (39,7%) и 3-е – рак яичников.
Среди мужчин в возрасте 15–19 лет 1-е место занимает рак яичка (87,8%), 2-е – рак мочевого пузыря (9,4%), 3-е – рак предстательной железы (2,3%). В возрастной группе 20–29 лет 1-е место занимает рак яичка (85,5%), 2-е – рак мочевого пузыря (11,9%) и 3-е – рак полового члена (1,3%). Среди мужчин 30–39 лет 1-е место занимает рак яичка (69%), 2-е – рак мочевого пузыря (23,9%), 3-е – рак полового члена (3,2%).
Показатели заболеваемости у женщин в целом выше, чем у мужчин, во всех возрастных группах за счет высокой заболеваемости РШМ и раком молочной железы. При распределении больных онкологическими заболеваниями репродуктивных органов в Российской Федерации в 2020 г. по полу женщин оказалось 9563 (89,9%), мужчин – 1080 (10,1), соотношение составило 8,9:1,0.
Обращает на себя внимание динамика изменения среднего возраста больных РШМ, в котором впервые в жизни установлен диагноз ЗНО. Так, если для всех ЗНО (в среднем) у женщин данный показатель с 2007 по 2020 г. постепенно возрастал с 62,5 до 64,0 года, то для РШМ он снизился на 5,5 года (с 57,5 года в 1993 г. до 52,5 года в 2020 г.) (рис. 3).
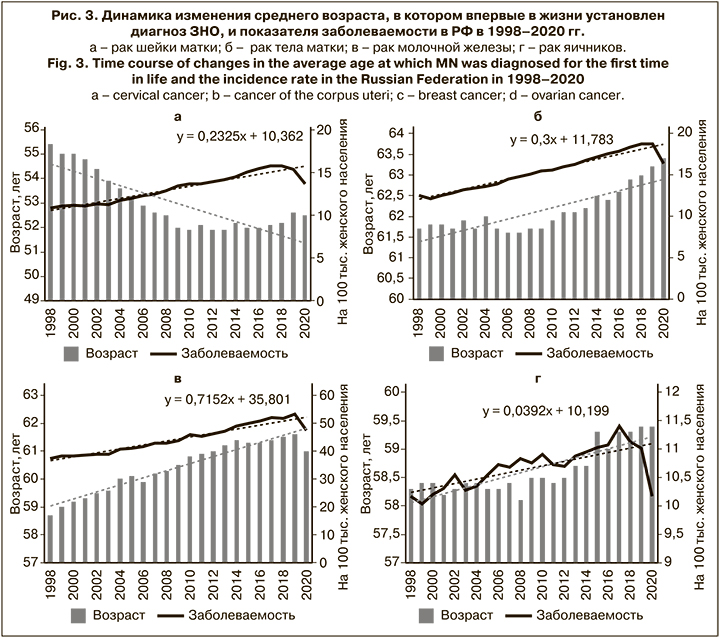
Таким образом, можно говорить о постепенном «омоложении» РШМ. РШМ выделяется на фоне других ЗНО у женщин возрастным распределением заболеваемости: если по всем ЗНО (в среднем) пик заболеваемости приходится на возраст 70–80 лет, то для РШМ он отмечается в 40–44 года.
Одной из главных причин заболеваемости ЗНО репродуктивных органов является высокая распространенность вируса папилломы человека (ВПЧ) среди молодого населения. Исходя из представленных данных по заболеваемости ЗНО в РФ за период 2011–2020 гг., на основании данных по ассоциации ВПЧ с патологическими изменениями в тканях [10] рассчитан ежегодный обобщенный показатель заболеваемости ВПЧ-ассоциированными новообразованиями репродуктивных органов в РФ среди населения в возрасте от 15 до 39 лет (табл. 1).
Обсуждение
Наблюдаемое в 2020 г. статистически достоверное снижение заболеваемости ЗНО по сравнению с 2019 г. может быть связано с пандемией COVID-19. Режим изоляции и «локдауны» препятствовали обращению к врачам граждан с неинфекционной патологией, снизились охват населения профилактическими осмотрами в рамках диспансеризации, а также диагностика и выявляемость онкологических заболеваний. Подобная ситуация в дальнейшем может привести к более позднему выявлению онкологических заболеваний, преобладанию первичных больных с III–IV стадиями, а также росту заболеваемости и смертности от ЗНО в последующие годы [11].
Снижение онкологической заболеваемости, связанное с пандемией COVID-19, отмечено и в других странах. Например, в Нидерландах в начале 2020 г. подобная тенденция наблюдалась практически по всем формам ЗНО [12]. Вынужденная временная приостановка скрининга рака молочной железы привела к снижению заболеваемости, однако после восстановления скрининговых программ в середине 2020 г. показатели вернулись к прежним значениям [13].
Что касается группы подростков и молодых людей, то наибольшая заболеваемость новообразованиями репродуктивных органов была выявлена среди лиц 30–39 лет, что может быть обусловлено не только прогрессом в диагностике, но и увеличением вероятности иметь определенный гинекологический и урологический анамнез к данному возрасту, увеличением воздействия таких факторов риска, как сопутствующие заболевания, длительный стаж курения, неправильное питание. Возможно, имеются и другие генетические, экологические и биологические факторы, изучение которых требует дальнейших исследований в расширенном масштабе.
Преобладание женщин – особенность структуры ЗНО в возрастной группе от 15 до 39 лет. РШМ и рак молочной железы вносят наибольший вклад в заболеваемость среди женщин. Основная причина неблагоприятных исходов у молодых женщин с раком молочной железы заключается в большей вероятности иметь генетическую предрасположенность к данной патологии, чем у женщин более старшего возраста, и, кроме того, у значительной части из них обнаруживаются отдаленные метастазы на момент постановки диагноза. Эти характеристики следует учитывать при разработке мероприятий по борьбе с ЗНО. Расширенный генетический скрининг может стать важной мерой в ранней диагностике рака молочной железы и снизить показатели заболеваемости и смертности в данной возрастной группе [14. 15].
Препятствием к снижению заболеваемости РШМ является высокая распространенность ВПЧ среди молодого населения. Национальная гендерно-нейтральная программа вакцинации против ВПЧ людей, ранее не инфицированных, может иметь значительный эффект в снижении тенденций заболеваемости и смертности [16].
Для сохранения репродуктивного потенциала молодых женщин и с учетом высокой распространенности папилломавирусной инфекции, а также РШМ в Москве и Московской области вступил в силу приказ «Об утверждении регионального календаря профилактических прививок», согласно которому вакцинопрофилактика против папилломавирусной инфекции проводится девочкам-подросткам. Москва и Московская область стали одними из первых регионов Российской Федерации по проведению масштабного проекта по иммунизации против РШМ, где была принята областная программа «Вакцинопрофилактика онкологических заболеваний, вызываемых вирусом папилломы человека» [17].
Что касается наиболее частой патологии у мужчин, по данным Национального института рака (National Cancer Institute, NCI), показатели заболеваемости раком яичек растут во всем мире, что делает его наиболее распространенным злокачественным новообразованием у мужчин в возрасте от 15 до 40 лет. Нет известного способа профилактики рака яичек, в связи с этим медицинские работники должны повышать осведомленность населения и раннее выявление данной патологии [18, 19].
Повышение осведомленности об онкологических заболеваниях, продвижение современных скрининговых программ, увеличение охвата вакцинацией и снижение влияния других факторов риска имеют важное значение, учитывая, что значительную часть случаев рака среди подростков и молодых людей можно предотвратить [20].
Заключение
Тренды заболеваемости и смертности от ЗНО репродуктивных органов в разных возрастных группах 15–19, 20–29 и 30–39 лет позволили дать характеристику и оценку общей тенденции, которая показала рост заболеваемости, отсутствие снижения смертности до 2019 г. и снижение показателей в 2020 г. в связи с пандемией COVID-19. Также увеличились заболеваемость и смертность в зависимости от возраста. Стратификация по возрастным группам позволила провести более подробную оценку возрастных тенденций в популяции молодых людей, что является преимуществом исследования. Полученные данные подчеркивают необходимость сосредоточить внимание на подростках и молодых людях при разработке программ борьбы с онкологическими заболеваниями. Эти действия будут иметь важное значение для улучшения демографических показателей в стране.