Профилактика инфекций, в области хирургического вмешательства (ИОХВ) остается одной из актуальных проблем современной медицины [1–5]. Одним из условий обеспечения эффективной борьбы с ИОХВ является применение антибактериальных препаратов в профилактических целях. Антибактериальная профилактика значительно снижает частоту послеоперационных инфекционных осложнений, поэтому широко используется при оперативных вмешательствах [6–9]. Ее проведение научно обоснованно при конкретных видах хирургических операций с учетом сопутствующей патологии. При назначении антибактериальных препаратов следует учитывать как пользу, так и возможный риск, связанный с неблагоприятными последствиями их применения: формирование резистентных штаммов микроорганизмов, влияние на бактериальную флору кишечника, необоснованные финансовые потери [10, 11]. В связи с этим рациональное и эффективное применение антибактериальных препаратов возможно исключительно при совместной работе клинического фармаколога, лечащего врача, врача-эпидемиолога и врача-бактериолога медицинской организации.
Необходимо отметить, что даже при комбинированной антибактериальной профилактике и неуместно раннем назначении антибиотиков резерва проблема ИОХВ радикально не решается [12]. Многие авторы сходятся во мнении, что не все послеоперационные инфекционно-воспалительные осложнения можно предотвратить, так как все профилактические мероприятия направлены на экзогенные источники инфекций и не учитывают другие факторы развития инфекционных процессов: эндогенные инфекции, реакцию организма на инфекционный агент и вирулентность патогена [13,14].
Исследования показали, что от 10 до 70% всех инфекций, связанных с оказанием медицинской помощи, и от 26 до 60% ИОХВ можно предотвратить. [15].
«Предотвратимость» инфекций в области хирургического вмешательства при проведении антибактериальной профилактики
Антибактериальная профилактика, назначаемая в эмпирическом режиме, не направлена на уничтожение конкретных микроорганизмов. При этом антибиотики, в отличие от антисептиков, имеют избирательность, и для проведения адекватного и обоснованного с точки зрения фармакологии выбора препарата нужно четко представлять, какое осложнение мы хотим предотвратить. Когда определены потенциально возможное осложнение и предполагаемый возбудитель, тогда и будет обоснован выбор лекарственного средства [16–18]. Разумеется, это должно быть наиболее частое, актуальное, а главное, предотвратимое осложнение.
С точки зрения антибиотикопрофилактики лишь определенную часть ИОХВ возможно предотвратить. Таким образом, ИОХВ могут быть предотвратимыми и непредотвратимыми [18,19].
Термин «предотвратимая антибиотикопрофилактикой ИОХВ» можно определить как ИОХВ, возникшая в результате предотвратимых причин при использовании антибактериальных препаратов в профилактических целях, исходя из современных знаний и практики, с учетом исходного состояния пациента.
Примером такого инфекционного осложнения можно считать нагноение раны у больного, перенесшего «чистую» операцию. Возбудитель предсказуем, технически правильно назначенная антибактериальная профилактика в данной ситуации существенно снижает риски.
Термин «непредотвратимая антибиотикопрофилактикой ИОХВ» можно определить, как ИОХВ, возникшая в результате причин, на которые действие применяемых антибактериальных препаратов в профилактических целях не распространяется. Спрогнозировать такие осложнения невозможно, и они не зависят от организации профилактических мероприятий.
Примером непредотвратимого антибиотикопрофилактикой ИОХВ можно считать перитонит вследствие несостоятельности межкишечного анастомоза, перфорации полого органа, нарушения общей и местной гемодинамики; холангит или пиелонефрит в условиях неадекватной функции дренажей. Организация профилактических и противоэпидемических мероприятий, а также антибактериальная профилактика не смогут повлиять на развитие таких осложнений. Кроме того, воспалительным осложнением, непредотвратимым посредством антибактериальной профилактики, асептики и антисептики, должен считаться острый послеоперационный панкреатит, при котором патологический процесс практически всегда изначально носит характер асептического воспаления, а инфекционный компонент присоединяется позднее.
Цель нашего исследования – определение частоты развития ИОХВ, которые возможно предотвратить, используя антибактериальные препараты в профилактических целях.
Материалы и методы
Проведен ретроспективный эпидемиологический анализ работы хирургической службы ГБУЗ «Городская клиническая больница им. Д.Д. Плетнева» Департамента здравоохранения города Москвы в период 2015–2017 гг. Проанализированы исходы 37 944 оперативных вмешательств у пациентов, находившихся на стационарном лечении.
В зависимости от профиля и вида оперативного вмешательства хирургические отделения объединены в 2 группы – урологические отделения и отделения абдоминальной хирургии с коечным фондом по 180 коек.
В 1-ю группу включены 3 урологических отделения, где пациентам оказывают урологическую помощь в экстренном и плановом порядке. В отделениях выполняются все виды эндоскопических и лапароскопических оперативных вмешательств, реконструктивные операции мочеполовой системы, микрохирургические операции, оперативное лечение недержания мочи, дистанционное разрушение камней мочеточника, малоинвазивная диагностика и лечение урологических заболеваний на мочевом пузыре, мочеточниках и лоханке, мочеиспускательном канале и предстательной железе. В эту группу входит отделение, оказывающее лечебно-хирургическую помощь больным онкоурологического профиля. Практически все операции проводятся с применением современных ригидных и гибких эндоскопов и видеоэндоскопов.
Во 2-ю группу включены 4 хирургических отделения:
- отделение для оказания экстренной и плановой хирургической помощи пациентам с заболеваниями пищеварительной системы, где проводятся оперативные вмешательства на желудке и двенадцатиперстной кишке, печени, поджелудочной железе, селезенке, кишечнике;
- онкохирургические отделения для оказания плановой хирургической помощи, где выполняют оперативные вмешательства при колоректальном раке, опухоли пищевода, желудка, тонкой и толстой кишки, билиопанкреатодуоденальной зоны и забрюшинного пространства. В отделениях проводятся малоинвазивные оперативные вмешательства, в том числе эндоскопическое стентирование пищевода, желудка, 12-перстной кишки при нерезектабельных опухолях.
Регистрацию ИОХВ проводили в соответствии со стандартным определением случая ИОХВ. По результатам анализа выявлены 152 ИОХВ у 146 пациентов, из них 6 пациентам проводили по 2 оперативных вмешательства. Информацию о послеоперационных инфекционно-воспалительных осложнениях брали из медицинских карт стационарного больного (форма №003/у), журнала учета инфекционных заболеваний формы № 060/у, консультативных журналов клинического фармаколога.
Диагнозы ИОХВ были распределены на 3 группы согласно критериям Национальной системы наблюдения за нозокомиальными инфекциями (National Nosocomial Infection Surveillance – NNIS) центров по контролю и профилактике заболеваний США (Centers for Disease Control and Prevention – CDC): 1-я – поверхностные ИОХВ разреза, 2-я – глубокие ИОХВ разреза, 3-я – ИОХВ органа/полости, вовлекающий орган или полость [19].
Поверхностные инфекции разреза представлены нагноением и диастазом послеоперационной раны; глубокие ИОХВ разреза представлены абсцессом, флегмоной послеоперационной раны, эвентрацией в послеоперационную рану; ИОХВ органа/полости представлены перитонитом, пиелонефритом, несостоятельностью межкишечного анастомоза и абсцессами поддиафрагмальным и забрюшинного пространства.
Все ИОХВ стратифицированы при помощи индекса риска NNIS. Методика предложена NNIS в 1970 г. [20]. Индекс риска NNIS рассчитывается в баллах от 0 до 3 и основан на следующих факторах риска:
- Предоперационная оценка тяжести состояния пациента по шкале ASA (Американского общества анестезиологов) 3 и более баллов.
- Контаминированная или «грязная» операция. Для оценки чистоты операционной раны использована классификация хирургических ран по степени микробной контаминации Altemeier [21].
- Превышение длительности операции более 75-го перцентиля продолжительности всех выполненных операций данного типа.
Каждый из трех параметров оценивается качественно: 0 баллов при отсутствии фактора риска и 1 балл при его наличии. Индекс риска NNIS представляет собой сумму этих баллов [10, 21].
Истории болезней пациентов с диагнозом ИОХВ проанализированы клиническим фармакологом и врачом-эпидемиологом медицинской организации с точки зрения возможности предотвратить каждый из зарегистрированных случаев ИОХВ при помощи организации профилактических мероприятий и проведения антибиотикопрофилактики. По результатам анализа все случаи ИОХВ распределены на предотвратимые и непредотвратимые с учетом вышеизложенных определений.
Материалы исследования были подвергнуты статистической обработке с использованием методов параметрического и непараметрического анализа. Накопление, корректировку, систематизацию исходной информации и визуализацию полученных результатов осуществляли в электронных таблицах Microsoft Office Excel 2016. Статистический анализ проводили с использованием программы IBM SPSS Statistics v.23 (разработчик – IBM Corporation).
Номинальные данные описывали с указанием абсолютных значений и процентных долей и сравнивали, используя χ2-критерий Пирсона.
Для оценки диагностической значимости количественных признаков при прогнозировании развития ИОХВ, в том числе вероятности развития ИОХВ в двух группах наблюдения в зависимости от группы риска NNIS, рассчитанной с помощью регрессионной модели, применяли метод анализа ROC-кривых. С его помощью пациенты классифицированы по степени риска исхода c наилучшим сочетанием чувствительности и специфичности. Качество прогностической модели оценивали, исходя из значений площади под ROC-кривой со стандартной ошибкой и 95% доверительным интервалом (95% ДИ) и уровня статистической значимости. Различия считали статистически достоверными при р < 0,001.
Результаты
В отделениях абдоминальной хирургии зарегистрировано 103 случая ИОХВ, что составило 67,8% всех зарегистрированных ИОХВ.
При стратификации ИОХВ с помощью индекса риска NNIS установлено:
- в 78,5% случаев операционные раны расценивались как контаминированные и были оценены в 1 балл;
- 96% пациентов относились к III классу по шкале ASA. Все случаи оценены в 1 балл.
- среди зарегистрированных ИОХВ в 52% случаев отмечено превышение длительности проведения операции в соответствии с 75-м перцентилем продолжительности всех выполненных операций данного типа, что оценено в 1 балл.
Получены сводные данные по частоте развития ИОХВ в соответствии с риском их возникновения, из которых видно, что в 88,3% ИОХВ в отделениях абдоминальной хирургии имеют риск развития 2 и 3 балла (48 и 43 случаев ИОХВ соответственно). Индекс риска NNIS, равный 1 баллу, имели 12 (11,7%) ИОХВ.
Среди ИОХВ преобладали инфекции органа/полости (51,5%), из них послеоперационные перитониты и абсцессы составили 75,5 и 11,2% соответственно. Поверхностные ИОХВ (34%) были представлены нагноением и диастазом послеоперационной раны. Глубокие ИОХВ разреза составили 14,5% и были представлены абсцессом и флегмоной послеоперационного рубца, эвентрацией в послеоперационную рану.
Выявлено 27 (26%) случаев ИОХВ, которые возможно было предотвратить при помощи периоперационной антибиотикопрофилактики. К ним отнесены нагноения и диастазы послеоперационной раны и абсцессы у пациентов без отягощенного анамнеза и сопутствующих патологий. 23 ИОХВ относились к поверхностным и 4 – к глубоким ИОХВ разреза. К предотвратимым относились 7 случаев ИОХВ с индексом риска NNIS, равным 1 баллу, и 20 случаев с индексом риска NNIS, равным 2 баллам.
76 (74%) случаев отнесли к группе непредотвратимых антибиотикопрофилактикой ИОХВ: перитониты и несостоятельность межкишечного анастомоза (47 случаев), эвентрации послеоперационной раны (8), абсцессы подпеченочного пространства и ложа желчного пузыря (6), дуоденальные свищи (2), флегмоны послеоперационной раны (2), а также нагноения послеоперационной раны и диастазы у пациентов с тяжелыми сопутствующими заболеваниями: субкомпенсированным и декомпенсированным сахарным диабетом (6), недостаточностью кровообращения (3), дыхательной недостаточностью (2).
По локализации развития в группе непредотвратимых ИОХВ преобладали осложнения органа или полости (69%). По индексу риска NNIS случаи с 2 и 3 баллами составили 57%, с 1 баллом – 43%.
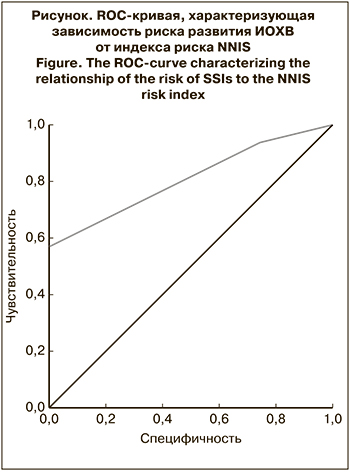 Частота развития непредотвратимых ИОХВ среди пациентов с индексом риска NNIS, равным 1 баллу, составляла 41,7%, среди пациентов с индексом риска 2–3 балла – 78,0%. Различия частоты развития непредотвратимых ИОХВ в зависимости от индекса риска NNIS статистически значимы (р = 0,13). Шансы развития непредотвратимых ИОХВ среди пациентов с индексом риска 2–3 балла в 4,97 раза выше, чем среди пациентов с индексом риска, равным 1 баллу (ОШ = 4,97; 95% ДИ 1,43–17,4). Различия были статистически значимыми (р < 0,001). Оценивая зависимость развития ИОХВ в отделениях абдоминальной хирургии от группы риска NNIS, мы получили следующую ROC-кривую (см. рисунок).
Частота развития непредотвратимых ИОХВ среди пациентов с индексом риска NNIS, равным 1 баллу, составляла 41,7%, среди пациентов с индексом риска 2–3 балла – 78,0%. Различия частоты развития непредотвратимых ИОХВ в зависимости от индекса риска NNIS статистически значимы (р = 0,13). Шансы развития непредотвратимых ИОХВ среди пациентов с индексом риска 2–3 балла в 4,97 раза выше, чем среди пациентов с индексом риска, равным 1 баллу (ОШ = 4,97; 95% ДИ 1,43–17,4). Различия были статистически значимыми (р < 0,001). Оценивая зависимость развития ИОХВ в отделениях абдоминальной хирургии от группы риска NNIS, мы получили следующую ROC-кривую (см. рисунок).
Площадь под ROC-кривой, характеризующей взаимосвязь прогноза развития ИОХВ и индекса риска NNIS, составила 0,806 ± 0,042 (95% ДИ 0,725–0,888). Полученная модель была статистически значимой (p < 0,001). Пороговое значение индекса риска NNIS в точке cut-off равно 2,5 балла. При индексе риска, равном или превышающем это значение, прогнозировался высокий риск развития ИОХВ.
Чувствительность и специфичность метода составили 93,4 и 74,1% соответственно.
В урологических отделениях зарегистрировано 49 (32,2%) случаев ИОХВ. При стратификации ИОХВ в соответствии с индексом риска NNIS установлено:
- в 38,7% случаев операционные раны расценивалось как контаминированные и были оценены в 1 балл;
- 63% пациентов относились к III классу по шкале ASA. Все случаи оценены в 1 балл;
- среди зарегистрированных ИОХВ в 75% случаев отмечено превышение длительности проведения операции в соответствии с 75-м перцентилем продолжительности всех выполненных операций данного типа, что оценено в 1 балл.
В урологических отделениях ИОХВ с индексом риска NNIS, равным 1–3 баллам, распределялись равномерно и составляли от 32,7 до 34,7%.
В отделениях зарегистрировано по 22 (45%) случая поверхностных ИОХВ и инфекций органа/полости. К поверхностным ИОХВ относили нагноения и диастаз послеоперационной раны. Инфекции органа/полости были представлены в основном пиелонефритом и абсцессом забрюшинного пространства, которые развились в послеоперационном периоде. Глубокие ИОХВ разреза, представленные флегмоной послеоперационного рубца и эвентрацией в послеоперационную рану, составили 10%.
В урологических отделениях 11 (22,5%) случаев ИОХВ были оценены как предотвратимые антибиотикопрофилактикой: нагноения и диастазы послеоперационной раны. Все ИОХВ относились к поверхностным ИОХВ разреза и имели индекс риска NNIS, равный 1 баллу.
К непредотвратимым антибиотикопрофилактикой ИОХВ отнесли 38 (77,5%) случаев: пиелонефриты на фоне неадекватной функции дренажа (7 случаев), абсцессы забрюшинного пространства (9) и перитониты (4), а также 18 случаев нагноений послеоперационной раны и диастазов у пациентов с тяжелыми сопутствующими заболеваниями в виде субкомпенсированного и декомпенсированного сахарного диабета.
В урологических отделениях в группе непредотвратимых ИОХВ по локализации развития преобладали осложнения органа либо полости (58%). Индекс риска NNIS был равен 1 баллу в 55% случаев, 2–3 баллам – в 45%. Частота развития непредотвратимых ИОХВ среди пациентов с индексом риска NNIS, равным 1 баллу, составляла 68,8%, с индексом риска 2–3 балла – 81,8%. Различия частоты развития непредотвратимых ИОХВ в зависимости от индекса риска NNIS статистически не значимы (р = 0,4). Шансы развития непредотвратимых ИОХВ у пациентов с индексом риска 2–3 балла в 2,05 раза выше, чем у пациентов с индексом риска, равным 1 баллу (ОШ = 2,05; 95% ДИ 1,19–152,2). Различия были статистически значимыми (р < 0,001).
При оценке взаимосвязи риска развития ИОХВ и индекса риска NNIS методом анализа ROC-кривых получена статистически незначимая модель (р > 0,001). Таким образом, отсутствует статистически значимая связь между риском развития ИОХВ и показателем индекса риска NNIS.
Обсуждение
Согласно современной нормативной базе, любое клинически выраженное заболевание микробного происхождения, которое поражает больного в результате его поступления в стационар или обращения за медицинской помощью, считается инфекцией, связанной с оказанием медицинской помощи.
К внутрибольничным послеоперационным инфекциям относятся заболевания, возникающие в течение 30 дней после оперативного вмешательства, а при наличии имплантата в месте операции – до 1 года1. При этом надо понимать, что очень часто ни усилия эпидемиолога, ни антибактериальная профилактика не имеют никакого отношения к оперативной технике хирурга, репаративной способности тканей пациента и его внимательности по отношению к дренажам [22]. Часть инфекций, связанных с оказанием медицинской помощи, предотвратить очень сложно, так как эти осложнения трудно предсказуемы, эффект от профилактических мероприятий слабый, нерегулярный или вовсе отсутствует. Предотвратимые осложнения могут с достаточной для клинического применения вероятностью быть предсказаны, их риск может быть существенно снижен посредством профилактических мероприятий [23].
Надо отметить, что часть непредотвратимых осложнений реализуется многоступенчато. Например, пациент получил послеоперационную стрессовую язву, которая осложнилась перитонитом. Можно предположить несоблюдение методик профилактики стрессовых язв или тромбоэмболических осложнений, хотя и их эффективность далеко не абсолютна. Но антибактериальная профилактика здесь ничего не решает, равно как и асептика с антисептикой.
Сложен вопрос с сопутствующими заболеваниями. Тяжелые и декомпенсированные сопутствующие заболевания увеличивают риск послеоперационных инфекционно-воспалительных заболеваний как минимум по двум механизмам. Один из них – иммунодефицит. Кроме очевидных причин, таких как ВИЧ-инфекция, генетически обусловленная иммунная недостаточность (первичный иммунодефицит), иммуносупрессивная терапия аутоимунных заболеваний, состояние после трансплантации органов, существует обширный круг заболеваний, способных спровоцировать клинически значимый вторичный иммунодефицит. Классический пример – сахарный диабет, особенно декомпенсированный. Кроме того, иммунодефицитом сопровождается хроническая почечная недостаточность (такие пациенты нередко встречаются в урологических отделениях), печеночная недостаточность (декомпенсированные циррозы печени), практически любая мальабсорбция (даже не приведшая к явному дефициту массы тела). Антибактериальная профилактика у этих пациентов проводится по расширенным показаниям, более активно и длительно. Однако вряд ли ее результаты целесообразно сравнивать с аналогичными результатами, полученными в группе больных с условно сохранной иммунной системой.
Второй механизм, увеличивающий риски инфекционно-воспалительных осложнений, – ишемия. Он менее значим, так как при поздних стадиях недостаточности кровообращения обширные оперативные вмешательства не практикуются из-за высокого операционно-анестезиологического риска. Тем не менее случаи реализации риска инфекционного процесса в ране целесообразно признать непредотвратимыми.
Вполне очевидно, что для каждой хирургической специальности распределение послеоперационных инфекционно-воспалительных осложнений будет иметь некоторый процент специфичности. Вряд ли правильно требовать от специалиста по хирургии печени усилий по профилактике простатита.
На наш взгляд, основной целью антибактериальной профилактики при операциях на коже и мягких тканях, органах желудочно-кишечного тракта, сосудах должно служить предотвращение воспалительного процесса в области операции – воспаления послеоперационной раны. Причем это может быть как классическое нагноение в области послеоперационного шва, так и глубокий воспалительный процесс, например, межкишечный абсцесс при операции на кишечнике. Отдельным вариантом воспаления послеоперационной раны может считаться перипротезная инфекция.
При оперативных вмешательствах на печени и желчных путях дополнительной целью профилактики может служить холангит. Однако это дополнение не отражается на выборе лекарственного препарата.
Все остальные варианты послеоперационных инфекционно-воспалительных осложнений целесообразно отнести к осложнениям непредотвратимым: всевозможные последствия несостоятельности анастомозов, перфорации полого органа, нарушения общей и местной гемодинамики. Кроме того, непредотвратимым посредством антибактериальной профилактики, асептики и антисептики воспалительным осложнением должен считаться острый послеоперационный панкреатит, при котором патологический процесс практически всегда изначально носит характер асептического воспаления, а инфекционный компонент присоединяется позднее.
Несколько особняком стоит урология. При операциях на органах мочеполовой системы цель антибактериальной профилактики – предотвращение инфекционно-воспалительного процесса в оперируемом органе: почке, простате, уретре, кавернозных телах полового члена. Нагноение послеоперационной раны в качестве основной цели антибактериальной профилактика сохраняется лишь в тех нечастых для урологии ситуациях, когда в ходе вмешательства не вскрывается просвет мочевых путей.
Полученные нами данные могут использовать как врачи-эпидемиологи для организации профилактических и противоэпидемических мероприятий, принятия управленческих решений по отдельным лечебным отделениям и стационару в целом, так и клинические фармакологи для оценки эффективности проведения антибактериальной профилактики и ее корректировки.
Выводы
- Разработанный метод распределения ИОХВ на предотвратимые и непредотвратимые проведением антибиотикопрофилактики показал, что как в отделениях абдоминальной хирургии, так и в урологических отделениях преобладали непредотвратимые ИОХВ, которые составили 77,5 и 74% соответственно.
- Распределение ИОХВ на предотвратимые/непредотвратимые является критерием эффективности проводимой антибиотикопрофилактики. Если преобладают предотвратимые ИОХВ, значит антибиотикопрофилактика проводится не в полном объеме, и необходимо оценить сроки и схемы ее проведения. В случае преобладания непредотвратимых осложнений можно сделать вывод, что антибиотикопрофилактика проводятся корректно. Данное утверждение возможно при соблюдении общеизвестных мер профилактики ИОХВ, таких как дезинфекционно-стерилизационный режим, соблюдение асептики и антисептики.
- Все пациенты с ИОХВ имели один и более факторов риска развития осложнений. При этом риск развития ИОХВ, равный 2–3 баллам, имели 88% пациентов отделений абдоминальной хирургии. В урологических отделениях ИОХВ с индексом риска NNIS, равным 1–3 баллам, распределялись равномерно и составили от 32,7 до 34,7%.
- У пациентов отделений абдоминальной хирургии и урологии шансы развития непредотвратимых ИОХВ при индексе риска NNIS, равном 2 и 3 баллам, увеличивались соответственно в 4,97 (ОШ = 4,97; 95% ДИ 1,43–17,4) и 2,05 раза (ОШ = 2,05; 95% ДИ 1,19–152,2). Различия были статистически значимыми (р < 0,001).
- В результате оценки диагностической значимости количественных признаков при прогнозировании развития ИОХВ с помощью анализа ROC-кривых установлено, что в отделениях абдоминальной хирургии при индексе риска NNIS, превышающем 2 балла, прогнозировался высокий риск развития ИОХВ. В урологических отделениях отсутствовала статистически значимая связь между риском развития ИОХВ и показателем индекса риска NNIS.