Необоснованная госпитализация в противотуберкулезные отделения является относительно редким явлением, поскольку поэтапная диагностика туберкулеза (ТБ), начиная с лечебных учреждений общей лечебной сети и заканчивая обследованием у фтизиатра перед направлением в стационарное отделение, обеспечивает надежную верификацию диагноза. Помещение пациента в противотуберкулезный диспансер предполагает, прежде всего, обеспечение качественного лечения, а не проведение доступных в общей лечебной сети диагностических процедур для уточнения диагноза. Вместе с тем в клинической практике иногда возникают ситуации, когда в силу тех или иных причин на догоспитальном этапе ошибочно диагностируют активный ТБ и направляют больного в специализированное отделение. Гипердиагностику ТБ выделяют как одну из главных диагностических ошибок при патологических изменениях в легких, что обусловлено недостаточным анализом анамнестических данных, неправильной трактовкой рентгенологических изменений в легких, отсутствием возможности выполнить компьютерную томографию, неполным микроскопическим исследованием мокроты, отсутствием этиологической и морфологической верификации диагноза [1–3]. В результате частота случаев гипердиагностики ТБ в специализированных отделениях может достигать 30,7%, а назначаемое противотуберкулезное лечение является неоправданным, способствует развитию побочных реакций и увеличивает сроки нахождения больного в стационаре [2–4]. В таких ситуациях создается реальная угроза суперинфекции, что особенно опасно для ВИЧ-инфицированных лиц в силу наличия у них различной степени выраженности Т-клеточного иммунодефицита.
Цель исследования – анализ причин расхождения предварительного и окончательного клинических диагнозов в условиях противотуберкулезного стационара и определение путей повышения точности диагностики.
Материалы и методы
Проведен ретроспективный анализ 69 медицинских карт стационарных больных, которые находились на лечении в легочно-туберкулезном отделении Республиканской клинической туберкулезной больницы (РКТБ) Донецка в 2014–2018 гг. и у которых после проведения дополнительного обследования активный ТБ был исключен. Больные поступали в туберкулезно-легочное отделение для взрослых, рассчитанное на 60 коек и предназначенное для оказания квалифицированной лечебно-диагностической помощи больным ТБ легких с деструкцией, а также для диагностики и лечения всех случаев туберкулезного менингоэнцефалита в Республике. С учетом большого количества пациентов с коинфекцией ТБ/ВИЧ и существенного влияния ВИЧ-инфекции на клинико-лабораторную картину ТБ, больные были разделены на 2 группы: в 1-ю были включены ВИЧ-инфицированные пациенты (п = 31), во 2-ю – ВИЧ-негативные (п = 38). В обеих группах преобладали мужчины: 17 и 21 соответственно, средний возраст составлял 42,3 ± 1,8 и 57,8 ± 2,4 года, медианы койко/дней пребывания в стационаре – 10 и 11.
Всем пациентам проводили рутинное лабораторное обследование. Для выявления бактериовыделения выполняли микроскопию мазков мокроты на наличие кислотоустойчивых бактерий (КУБ), посев на жидкую среду Миддлбрука на аппарате BACTEC и твердую среду Левенштейна–Йенсена. При получении культуры проводили тест на лекарственную чувствительность микобактерий туберкулеза (МБТ) к противотуберкулезным препаратам 1-го и 2-го ряда. По показаниям применяли молекулярно-генетический метод GeenXpert MBT/Rif для выявления ДНК МБТ, спиральную компьютерную томографию (СКТ) органов грудной клетки и головы, фибробронхоскопию (ФБС) с изучением жидкости бронхоальвеолярного лаважа (БАЛ).
Статистический анализ проводили с использованием пакета MedStat [5]. При нормальном распределении определяли средние значения показателей; при распределении, отличном от нормального, данные представляли в виде медианы. Для качественных признаков рассчитывали частоту встречаемости.
Результаты
За период наблюдения из отделения выбыли 962 пациента, диагноз ТБ был исключен у 69 лиц, случаи ошибочной диагностики ТБ составил 7,2%.
В 1-й группе 24 (80,6%) больных поступали в отделение с предварительным диагнозом «ТБ легких» (см. таблицу).

Туберкулезный менингит подозревали у 15 (48,4%) пациентов, у 12 – в сочетании с ТБ легких и/или ТБ других локализаций и у 3 – изолированный. Также диагностировали одновременное специфическое поражение внутригрудных лимфоузлов (ВГЛУ), экссудативный плеврит, туберкулему головного мозга.
ТБ в анамнезе отмечали 9 (29,0%) человек, все они успешно закончили полный курс антимикобактериальной химиотерапии, при этом до поступления в наше отделение 6 человек наблюдались с остаточными изменениями менее года, и трое – в течение 8, 5 и 3 лет.
На догоспитальном этапе микроскопию мазка мокроты на КУБ выполняли 15 из 24 больных с предполагаемым ТБ легких, у всех результат был отрицательным. Лечение пневмонии получали трое пациентов (см. таблицу). Двое больных были направлены на госпитализацию без рентгенограмм органов грудной клетки, у остальных лучевое обследование провели за 1–4 нед. до поступления в стационар. При наличии плеврального выпота диагностические пункции не выполняли.
Из 15 больных с предполагаемым туберкулезным менингитом на момент поступления у 10 (66,7%) отсутствовали менингеальные знаки. Перед госпитализацией МРТ (СКТ) головного мозга выполняли 5 больным, в 3 случаях выявили изменения, характерные для токсоплазмоза. Лечение токсоплазмоза никому назначено не было, причиной госпитализации в РКТБ послужило подозрение на сопутствующий ТБ из-за наличия патологии на рентгенограммах органов грудной клетки (диссеминация, увеличение ВГЛУ). Спинномозговую жидкость исследовали у 5 пациентов, изменений, характерных для туберкулезной этиологии менингита, выявлено не было.
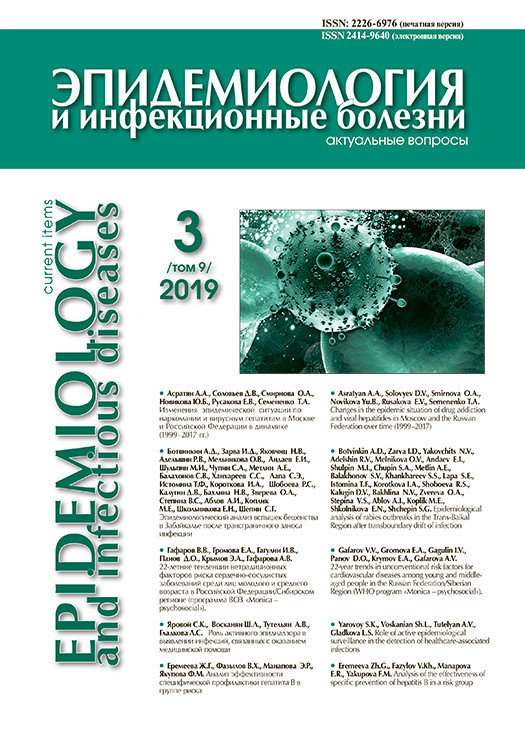
 После госпитализации в РКТБ в 1-й группе исследование мокроты микроскопическим, молекулярно-генетическим и культуральными методами было выполнено 20 (64,5%) пациентам, ни в одном случае МБТ обнаружены не были. Проведение всех доступных диагностических процедур позволило в период от 1 до 79 дней (медиана – 10 дней) установить окончательные клинические диагнозы, которые распределились следующим образом (рис. 1).
После госпитализации в РКТБ в 1-й группе исследование мокроты микроскопическим, молекулярно-генетическим и культуральными методами было выполнено 20 (64,5%) пациентам, ни в одном случае МБТ обнаружены не были. Проведение всех доступных диагностических процедур позволило в период от 1 до 79 дней (медиана – 10 дней) установить окончательные клинические диагнозы, которые распределились следующим образом (рис. 1).
В 1-й группе часто выявляли ВИЧ-ассоциированные заболевания нервной системы [6]. У 4 пациентов диагностировали ВИЧ-ассоциированную миелопатию, у 2 – кандидозный менингит, у 1 – криптококковый менингит и 1 пациенту установлен диагноз «кандидозный абсцесс головного мозга» (после оперативного лечения). Диагнозы «ВИЧ-ассоциированные заболевания нервной системы» и «токсоплазмоз головного мозга» выставили 13 из 15 больных, поступивших в отделение с подозрением на туберкулезный менингит. Оставшимся 2 пациентам были установлены диагнозы «острое нарушение церебрального кровообращения» и «глиобластома мозжечка». Для уточнения диагноза ведущее значение имела СКТ органов грудной клетки, которую выполнили 12 больным, в результате чего у 11 из них не было выявлено патологии в легких или изменений специфического характера, что в сочетании с изучением ликвора (у 6 пациентов) и анализа клинико-лабораторной картины заболевания в динамике позволило исключить туберкулезную этиологию поражения нервной системы в сроки от 1 до 39 дней (медиана – 6 дней).
В 8 случаях в качестве основного клинического диагноза выносили пневмонию, в том числе в 3 (37,5%) – пневмоцистную. Для уточнения диагноза в 3 случаях потребовалось только выполнить контрольное лучевое обследование и оценить динамику процесса на догоспитальном этапе, еще 2 пациентам провели лечение антибиотиками широкого спектра действия с последующим рентгенологическим контролем. Трое больных с первых дней пребывания в отделении получали терапию пневмоцистной пневмонии (бисептол, клиндамицин), в результате чего произошло полное рассасывание очагов в легких.
Онкологическая патология была представлена в 6 (85,7%) случаях карциноматозом легких, в 1 (14,3%) – глиобластомой мозжечка. Первичный рак легких как причину метастазирования регистрировали у 2 пациентов. Диагноз при жизни был установлен 2 пациентам из 7, в этом решающую роль сыграла СКТ органов грудной клетки; в остальных случаях диагноз был верифицирован по результатам аутопсии. Диагностика осложнялась тяжелым состоянием больных (четверо находились в отделении от 2 до 14 сут.).
Токсоплазмоз головного мозга был установлен как основной диагноз у 5 пациентов на основании исключения активного туберкулезного процесса (отсутствие характерных изменений ликвора и патологии в легких по данным СКТ), анализа результатов лучевого обследования головного мозга на догоспитальном этапе и в условиях нашей клиники.
Другие 3 случая ошибочной диагностики ТБ – острое нарушение мозгового кровообращения, тромбоэмболия легочной артерии и лекарственный пневмонит. В первых 2 случаях диагноз был подтвержден результатами аутопсии.
Клинический диагноз ТБ был установлен в отделении 5 (16,1%) ВИЧ-инфицированным пациентам, начата противотуберкулезная химиотерапия. Четверо пациентов умерли, при этом в 3 случаях длительность пробной терапии составляла 2, 11 и 14 дней и только в 1 случае специфическое лечение продолжалось в течение 47 дней. Результаты аутопсии не подтвердили наличия ТБ: у 3 больных выявили карциноматоз легких (рак легкого, матки и поджелудочной железы) и у 1 – глиобластому мозжечка. Еще у 1 больной после 33 дней приема противотуберкулезных препаратов на контрольной рентгенограмме отмечено полное рассасывание инфильтрации, что дало основание изменить диагноз на «внегоспитальную пневмонию».
Всего за период нахождения в отделении из 31 ВИЧ-инфицированного больного умерли 10, госпитальная летальность составила 32,3%. Предполагаемая нетуберкулезная этиология заболевания была подтверждена в 6 случаях, в 4 случаях диагнозы совпали («генерализованный кандидоз», «церебральный атеросклероз с острым нарушением мозгового кровообращения», «криптококковый менингит» и «рак легкого»), в 2 имело место расхождение (клинические диагнозы – «пневмония» и «рак желчного пузыря», патологоанатомические – соответственно «рак поджелудочной железы с метастазами в легкие» и «тромбоэмболия легочной артерии»).
Из 38 больных 2-й группы 35 (92,1%) поступили в отделение с предварительным диагнозом «ТБ легких», при этом превалировали инфильтративный и диссеминированный ТБ (см. таблицу). В остальных случаях фигурировали фиброзно-кавернозный и очаговый ТБ легких, ТБ бронха. У 1 больного предполагалось одновременное наличие туберкулезного менингита, у 7 – ТБ ВГЛУ и у 4 – экссудативного плеврита.
Ранее от ТБ лечились 2 (5,3 %) пациента, они закончили полный курс терапии за 1 год и 20 лет до поступления в наше отделение, еще 5 пациентам диагноз ТБ был выставлен непосредственно перед госпитализацией; на момент поступления эти больные получали противотуберкулезные препараты в течение от 1 до 6 мес.
Изучение полноты обследования на догоспитальном этапе показало, что рентгенографию и/или СКТ органов грудной клетки за 1–4 нед. до госпитализации выполняли всем пациентам. При подозрении на ТБ после рентгенологического обследования 27 (71,0%) пациентам проведено исследование на наличие КУБ методом микроскопии: мазка мокроты (21 человек), плеврального экссудата (1), осадка БАЛ (5). КУБ в мазках мокроты были обнаружены у 9 (42,8%) пациентов, в бронхолегочных смывах – у всех 5 (в том числе в 1 случае методом GeenXpert выявлена микобактериальная ДНК и устойчивость к рифампицину), в плевральном экссудате – у 1. Всего положительные результаты бактериологического исследования явились основанием для госпитализации в противотуберкулезный стационар 15 больных, что составило 39,5%.
На догоспитальном этапе от предполагаемой пневмонии получали терапию 20 (52,6%) больных, ее продолжительность составляла от 3 до 40 дней (медиана – 12 дней), 1 больного лечили от «хронического абсцесса» в течение 120 дней с малой эффективностью. Из антибиотиков наиболее часто использовали цефалоспорины и макролиды, 4 пациента получали фторхинолоны.
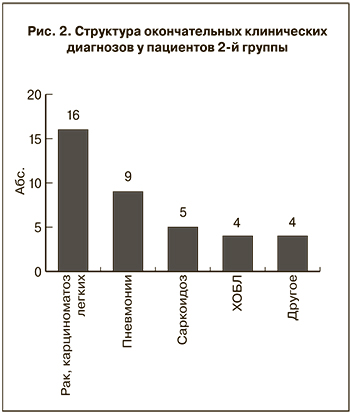 Во 2-й группе оценка динамики процесса и данных дополнительного обследования в условиях туберкулезного диспансера позволила установить окончательный диагноз в сроки от 4 до 170 дней (медиана – 11 дней). В результате выявлено, что наиболее часто встречалась онкологическая патология (рис. 2).
Во 2-й группе оценка динамики процесса и данных дополнительного обследования в условиях туберкулезного диспансера позволила установить окончательный диагноз в сроки от 4 до 170 дней (медиана – 11 дней). В результате выявлено, что наиболее часто встречалась онкологическая патология (рис. 2).
В 12 случаях диагностировали рак легкого с метастазами в легочную ткань и в 4 – карциноматоз легких (рак поджелудочной железы, лимфому, 2 случая опухоли неуточненной локализации). Все пациенты с онкологической патологией были старше 50 лет (медиана – 61 год), преобладали мужчины (10 человек). На момент госпитализации у 12 (75,0%) пациентов предварительным диагнозом был инфильтративный, у 3 (18,8%) – диссеминированный и у 1 пациента (6,2%) – фиброзно-кавернозный ТБ легких. На догоспитальном этапе 11 (68,8%) человек безуспешно лечились от предполагаемой пневмонии, диагностическая ФБС была выполнена 2 (12,5%) пациентам. Еще 2 провели СКТ органов грудной клетки. КУБ в мокроте были найдены у 5 (31,3%) больных. Никто из пациентов не был проконсультирован онкологом. В отделении уточнить характер патологии в легких помогло комплексное обследование. СКТ выполнена 8 (50,0%) пациентам (в 7 случаях – органов грудной клетки и в 1 случае – органов брюшной полости), выявившая источник карциноматоза. Диагностическая ФБС проведена также 8 (50,0%) пациентам, при этом в 4 случаях была визуализирована и подтверждена гистологическим исследованием опухоль верхнедолевого бронха. У 1 (6,2%) пациента после гистологического исследования надключичного лимфоузла выявлена неходжкинская лимфома, еще у 2 (12,5%) диагноз «рак легких» был выставлен на основании детального анализа рентгенологического архива в сравнении с данными контрольного лучевого обследования в условиях противотуберкулезного стационара. В итоге из 16 пациентов у 10 (62,5%) рак легкого был верифицирован в сроки до 20 дней, медиана – 8,5 дней (в 1 случае клинический диагноз подтвержден результатами аутопсии). В остальных 6 случаях потребовалось противотуберкулезное лечение в течение 35–170 дней, при этом 3 больным его провели на догоспитальном этапе и 3 пациентам назначили в РКТБ. Отрицательная рентгенологическая динамика процесса на этом фоне стала основанием для пересмотра диагноза и дополнительного обследования.
2-е место в структуре окончательных диагнозов у пациентов 2-й группы занимали внегоспитальные пневмонии (9 случаев). Все пациенты поступили в отделение с предварительным диагнозом «инфильтративный ТБ легких». Мокроту на наличие КУБ до госпитализации исследовали у 7 пациентов. На догоспитальном этапе лечение пневмонии получали 3 больных, у них же были выявлены КУБ: в 2 случаях – в бронхолегочных смывах, в 1 – в мазке мокроты, что послужило основанием для перевода в противотуберкулезный диспансер. В противотуберкулезном учреждении анализ клинико-лабораторной картины заболевания и контрольное рентгенологическое обследование позволили сразу исключить ТБ у 2 больных; 6 пациентам назначали антибиотики широкого спектра действия, после которых наступило полное (значительное) рассасывание инфильтрации в легких, и только в 1 случае потребовалась тест-терапия антимикобактериальными препаратами в течение 60 дней, после чего по результатам СКТ органов грудной клетки диагноз ТБ был снят. Бактериологическое обследование мокроты всеми методами ни в одном случае не выявило бактериовыделения.
Саркоидоз легких был диагностирован у 5 больных. При поступлении у всех рентгенологически определялись увеличенные ВГЛУ, диссеминация в легких; у 2 пациентов на догоспитальном этапе в мокроте обнаружены КУБ, в том числе в 1 случае – микобактериальная ДНК в бронхолегочном смыве методом GeenXpert. В условиях РКТБ исследование мокроты и бронхолегочных смывов всеми методами МБТ не выявило, все пациенты отказались от биопсии легкого. Диагноз «саркоидоз» выносили на основании наличия интерстициальных изменений, диссеминации и двустороннего увеличения внутригрудных лимфоузлов по данным СКТ органов грудной клетки, стабильности процесса при оценке клинико-рентгенологической динамики за период от 6 мес. до 1 года, отсутствия патологии при рутинном лабораторном обследовании. У 3 пациентов результаты пробы Манту с 2 ТЕ были отрицательными. В 1 случае методом ФБС выявили характерные для саркоидоза сосудистые изменения на слизистой оболочке бронхов. Бактериовыделения обнаружено не было. В результате ТБ легких был исключен в сроки от 8 до 13 дней.
У всех пациентов с окончательным диагнозом «хроническая обструктивная болезнь легких» (ХОБЛ, n = 4) на догоспитальном этапе были выявлены КУБ, в том числе у 2 – в бронхолегочных смывах. Рентгенологически изменения в легких определили у 1 пациента, он поступил в отделение с диагнозом «инфильтративный ТБ». У остальных лиц предварительным диагнозом был ТБ бронха. В отделении всем больным выполнена ФБС с исследованием БАЛ, бактериологическое исследование (микроскопия, выявление ДНК МБТ методом GeenXpert, посев на среды Левенштейна–Йенсена и Миддлбрука), СКТ органов грудной клетки. На основании отсутствия бактериовыделения, характерных для ТБ изменений на СКТ (в 1 случае выявлены множественные бронхоэктазы, в остальных – диффузный пневмосклероз, эмфизема, участки фиброза) ТБ был исключен в сроки от 8 до 10 дней (медиана – 9,5 дней).
Другие случаи неподтвержденных диагнозов ТБ были представлены ИБС с явлениями застойной сердечной недостаточности и плевральным выпотом, интерстициальным заболеванием легких (n = 2), раком поджелудочной железы с метастазами в головной мозг. Пациенты находились в отделении непродолжительный период – от 7 до 24 дней (медиана – 11,5 дней).
Всего из 38 пациентов 2-й группы в отделении умерли 3 (7,9%), в 2 случаях диагнозы совпали («внегоспитальная пневмония», «рак легкого»), в 1 случае диагноз был установлен по результатам аутопсии («рак поджелудочной железы с метастазами в головной мозг»), тогда как в отделении у больного был диагностирован системный облитерирующий тромбангиит.
Обсуждение
Согласно полученным результатам, за исследуемый период частота ошибочной диагностики ТБ составляла 7,2%, что было несколько ниже данных, приведенных в других исследованиях, в которых этот показатель колебался от 10,3% [7] до 30,7% [4]. Мы согласны с мнением О.В. Демиховой и соавт. [3], что одной из главных причин диагностических ошибок на догоспитальном этапе является неполное обследование. Так, ВИЧ-инфицированных пациентов в большинстве случаев направляли на госпитализацию в специализированный противотуберкулезный диспансер без выполнения всего объема стандартных диагностических процедур, предусмотренных протоколом. Создавалось впечатление, что наличие ВИЧ-инфекции являлось главным основанием выставить диагноз ТБ при упоминании о нем в анамнезе, появлении патологии на рентгенограммах органов грудной глетки и при наличии неврологической симптоматики. Среди ВИЧ-негативных пациентов основными причинами вынесения диагноза ТБ были отсутствие клинико-рентгенологического эффекта от неспецифической антибактериальной терапии и выявление КУБ в биологическом материале, преимущественно в мокроте.
Продолжительность пребывания в отделении 69 пациентов, госпитализированных с ошибочным диагнозом ТБ, составляла от 1 до 175 дней, (медиана – 11 дней). При этом у 44 (63,8%) больных для уточнения диагноза понадобилось 14 и менее дней (медиана – 7 дней). Ведущую роль в верификации диагноза, помимо бактериологического исследования, сыграли СКТ грудной полости (головы), неспецифическая антибактериальная терапия и/или контрольное лучевое обследование, детальное изучение клинико-лабораторной и рентгенологической картины заболевания в динамике, а также диагностическая ФБС, гистологическое изучение материалов биопсии. Очевидно, что выполнение указанных исследований в условиях общей лечебной сети позволило бы уточнить диагноз и избежать госпитализации в инфекционное туберкулезное отделение. Клинический диагноз ТБ был установлен 7 (10,1%) больным: 4 пациентам 1-й группы и 3 – 2-й. Им начали проводить противотуберкулезную химиотерапию.
Выявление КУБ в биологическом материале на догоспитальном этапе, не нашедшее своего подтверждения при обследовании в специализированной лаборатории, имело место только у пациентов 2-й группы и послужило причиной ошибочной госпитализации 15 (39,5%) человек. Доля ложноположительных результатов микроскопии мазка мокроты была выше, чем в исследованиях Ж.А. Лаушкиной и соавт. [7], где этот показатель составлял 7,3%. Очевидно, что положительные результаты микроскопии мокроты должны оцениваться в комплексе с результатами других бактериологических и молекулярно-генетических методов исследования. Так, N.P. Mnyambwa и соавт. [8] сообщают, что из 94 пациентов с положительным мазком и предварительным диагнозом ТБ легких у 6 (6,4%) были выявлены нетуберкулезные микобактерии, что позволило расценивать результаты микроскопии как ложноположительные, а у 60 (63,8%) случаи ТБ обозначили как неподтвержденные, поскольку культуральными и молекулярно-генетическими методами МБТ обнаружены не были. Пересмотр в референс-лаборатории РКТБ 6 образцов мокроты с положительным результатом бактериоскопии, выполненной в лабораториях общей лечебной сети, показал, что у 2 пациентов КУБ в препаратах отсутствовали, в 1 случае были представлены микобактериями, по своим внешним признакам и расположению в препарате не типичными для туберкулезных, и в 3 случаях были обнаружены однократно в малом количестве – не более 3–5 на 300 полей зрения. Последнее дало основание расценивать результаты как положительные, но не являющиеся следствием ТБ. Так, в группу больных с выявленными на догоспитальном этапе КУБ (n =15) вошли все 4 пациента с ХОБЛ (26,7%), 5 больных раком легкого с метастазами в легочную ткань (33,3%), 3 пациента с пневмониями (20,0%) и 2 – с саркоидозом (13,3%). В итоге высокий процент положительных результатов микроскопии мокроты мы объясняли попаданием в препарат нетуберкулезных микобактерий или МБТ из старых очагов у пациентов с деструктивными процессами в легких. Также не исключалось нарушение в некоторых случаях техники изготовления мазков. Особенно часто ложноположительные случаи обнаружения КУБ встречались при исследовании бронхолегочных смывов, что позволяет предполагать наличие контаминации биологического материала микобактериями даже при самой тщательной обработке фибробронхоскопов.
Выводы
- ВИЧ-инфицированных пациентов направляли на госпитализацию в специализированный противотуберкулезный диспансер без выполнения полного объема стандартных диагностических процедур, предусмотренных протоколом: из 24 больных с подозрением на ТБ легких исследование мокроты проводили у 15, а при наличии инфильтратов в легких у 8 пациентов лечение пневмонии было назначено только двоим. Из 15 пациентов с подозрением на туберкулезный менингит (менингоэнцефалит) спинномозговые пункции и лучевое обследование головного мозга выполнили 5 больным.
- Из 38 больных 2-й группы у 15 (39,5%) на догоспитальном этапе были выявлены КУБ, что стало основанием для госпитализации в противотуберкулезное отделение, но в дальнейшем не нашло подтверждения при обследовании в условиях специализированной лаборатории. Для улучшения качества диагностики в учреждениях общей лечебной сети следует направить усилия на повышение точности микроскопического исследования и предотвращение контаминации образцов биологического материала, что имеет особенное значение при исследовании бронхолегочных смывов.
- В условиях противотуберкулезного диспансера оценка клинической картины и динамики процесса на догоспитальном этапе, проведение компьютерной томографии, диагностической бронхоскопии, антибактериального неспецифического лечения с выполнением контрольного лучевого обследования позволило в короткие сроки (менее 2 нед.) уточнить диагноз у 63,8% пациентов. Для предотвращения необоснованной госпитализации в инфекционное противотуберкулезное отделение следует проводить более полное обследование пациентов в соответствии с протоколом на догоспитальном этапе.
- При наличии у ВИЧ-инфицированных больных с отрицательным результатом микроскопии мазка мокроты на КУБ клинико-рентгенологических признаков пневмонии, в том числе атипичной, лечение следует проводить в специализированных отделениях СПИД-центров с повторной консультацией фтизиатра в случае необходимости.